I'm late to this thread, but I want to echo Kitty's concern about that poor article by Cort. I'm concerned that many people who haven't been around long enough to see findings come and go might have made or might be making life-changing decisions based on an interpretation of an interpretation of findings that we can't know for sure will pan out to be true for even a subset of people with ME/CFS, let alone everyone with an ME/CFS diagnosis.
We should not assume that this is necessarily correct, or unfixable. We've seen people diagnosed with severe ME/CFS spontaneously recover a large amount of function. Even if the situation is bad, you may well not have what the people who were autopsied had.
I have been wondering that too.
I think we have to consider the possibility that the people who were in a position to donate their brains may not be representative of people with ME/CFS generally. I suspect that most of them underwent planned euthanasia. I may be wrong. But, if they did, and clearly most people with ME/CFS are not doing that, then that raises all sorts of possibilities.
Regarding the brain cortisol finding: we have had studies on cerebral spinal fluid and I'm pretty sure that abnormalities in cortisol levels in the brain have not been found. There may be some notes about that on the cortisol thread. Googling, it looks as though people who die difficult deaths, with severe injuries for example, have high levels of cortisol in their brains. People who have medicated deaths may well have much lower levels of cortisol in their brains.
People who decide that euthanasia is their best option may have been on certain drugs long term and other drugs at the time of their death. They may be more likely to have certain co-morbidities or even a primary illness that are different to what other people with an ME/CFS diagnosis have.
View attachment 30493
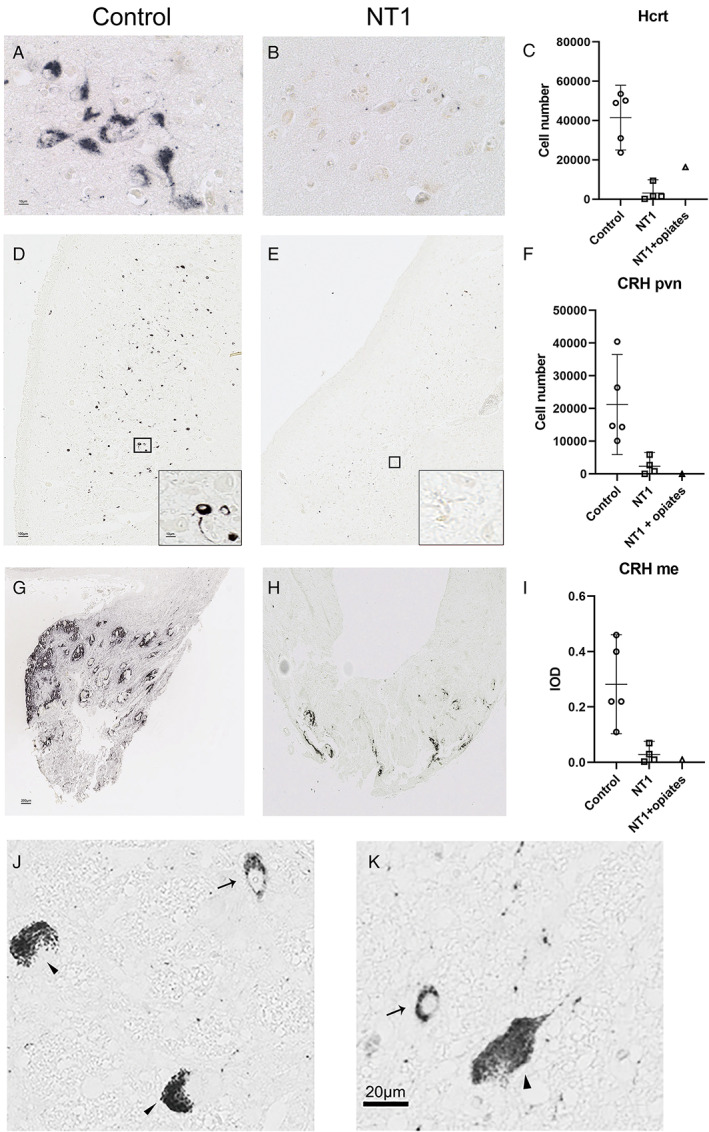
Mostly though, I look at that chart of the CRH cells and I find it hard to believe. These investigators specifically looked at this part of the brain because they believed that people with ME/CFS have hypocortisolism. They therefore approached this study expecting to find something like what they found. On average, we do not have hypocortisolism.
Given the uncertainties around ME/CFS diagnosis, I find it hard to believe that all of the 'ME/CFS' brain donors had exactly the same pathology, and yet the CRH neuron numbers are all so clustered close to zero. We know that biological tissue is often very variable, and yet, again, there is no variability in those results.
I think there are quite a range of consequences that we would expect to flow from an almost total lack of CRH neurons. I think there will be some data that we can use to test that idea.