ahimsa
Senior Member (Voting Rights)
Moved post
Editorial in The Michigan Daily:
Michigan Medicine needs to address post-viral illness
https://www.michigandaily.com/opinion/michigan-medicine-needs-to-address-post-viral-illness/
Very good op-ed piece, includes discussion of both ME/CFS and Long Covid.
Editorial in The Michigan Daily:
Michigan Medicine needs to address post-viral illness
https://www.michigandaily.com/opinion/michigan-medicine-needs-to-address-post-viral-illness/
Very good op-ed piece, includes discussion of both ME/CFS and Long Covid.
The Michigan Daily said:My name is Glenn Tucker and I live with a debilitating disease called myalgic encephalomyelitis, or ME for short. According to the Centers for Disease Control, “People with ME have overwhelming fatigue that is not improved by rest. ME may get worse after any activity, whether it’s physical or mental.” ME used to be called Chronic Fatigue Syndrome, a term many now find offensive, including some of the doctors that coined it. A 1996 study published in the American Journal of Medicine — and since corroborated multiple times — found that people with ME score lower on quality of life indices than people with cancer, heart disease, multiple sclerosis and diabetes.
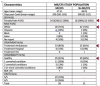
If you haven’t heard of ME, it’s not because it is a rare disease: before the pandemic an estimated 2 million Americans lived with ME, more than HIV/AIDS (1.2m), lupus (785k) and multiple sclerosis (486k). Nearly eighty percent of ME cases start with a viral infection. Seventy-five percent of people with ME are women, and 25% are bedridden, like me. I have been bedridden for nearly four years and sick for nearly eight. A 2008 study found that ME costs our nation’s economy between $17 billion and $24 billion in lost wages and medical expenses.
Last edited by a moderator: