rvallee
Senior Member (Voting Rights)
Integration of psychological care into a nontuberculous mycobacteria (NTM) program in the Southeastern United States: A retrospective cohort study
Therapeutic advances in respiratory disease
PubMed: https://pubmed.ncbi.nlm.nih.gov/41222255/
PDF: https://journals.sagepub.com/doi/pdf/10.1177/17534666251394479
Abstract
Background: Nontuberculous mycobacterial lung disease (NTM-LD) is a chronic infection of the lungs with a high symptom burden. NTM-LD treatment is typically long and complicated, which can impact quality of life and mental health. Increased support for psychological challenges is a priority for this population.
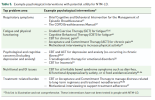
Objectives: We describe integrating psychological care into a multidisciplinary outpatient NTM program, patient characteristics, and results of patient-reported outcomes (PRO) screening (of depression, anxiety, fatigue, health-related quality of life, quality of life, and Top Problems).
Design: Retrospective observational cohort study design.
Methods: Processes and structure around psychology integration are described. Descriptive data obtained via retrospective chart review (IRB approved) are presented on patient sociodemographic factors, psychiatric medication and psychotherapy use, and results of PRO screenings with NTM-LD patients anticipated to start NTM antibiotic treatment or already on treatment. Relationships between variables were examined using nonparametric statistics.
Results: From 2020 to 2024, 175 patients with NTM-LD were screened. Patients were on average 65.7 ± 9.8 years old, female (74.2%), white (91.4%), and on Medicare (69.1%). On average, this group experienced a moderate degree of socioeconomic disadvantage; 94.9% of patients lived in areas with a mental health provider shortage, and 42.3% lived in medically underserved areas. Patients reported considerable rates of mild or higher depression (54.3%) and anxiety (32.0%). Many utilized psychiatric (52.6%) or pain (20.6%) medications, while engagement in psychotherapy was low (5.1%). Patients reported impacts on quality of life, fatigue, and health-related quality of life, and the most common Top Problems were: "Shortness of breath, Breathlessness, Getting winded," "Fatigue/Low energy," and "Cough/Choking."
Conclusion: A licensed psychologist was successfully integrated into the NTM program. The disparity between PRO results and psychotherapy engagement highlights a key opportunity for mental health interventions. Integrated psychological services may provide streamlined access to mental healthcare.
Therapeutic advances in respiratory disease
PubMed: https://pubmed.ncbi.nlm.nih.gov/41222255/
PDF: https://journals.sagepub.com/doi/pdf/10.1177/17534666251394479
Abstract
Background: Nontuberculous mycobacterial lung disease (NTM-LD) is a chronic infection of the lungs with a high symptom burden. NTM-LD treatment is typically long and complicated, which can impact quality of life and mental health. Increased support for psychological challenges is a priority for this population.
Objectives: We describe integrating psychological care into a multidisciplinary outpatient NTM program, patient characteristics, and results of patient-reported outcomes (PRO) screening (of depression, anxiety, fatigue, health-related quality of life, quality of life, and Top Problems).
Design: Retrospective observational cohort study design.
Methods: Processes and structure around psychology integration are described. Descriptive data obtained via retrospective chart review (IRB approved) are presented on patient sociodemographic factors, psychiatric medication and psychotherapy use, and results of PRO screenings with NTM-LD patients anticipated to start NTM antibiotic treatment or already on treatment. Relationships between variables were examined using nonparametric statistics.
Results: From 2020 to 2024, 175 patients with NTM-LD were screened. Patients were on average 65.7 ± 9.8 years old, female (74.2%), white (91.4%), and on Medicare (69.1%). On average, this group experienced a moderate degree of socioeconomic disadvantage; 94.9% of patients lived in areas with a mental health provider shortage, and 42.3% lived in medically underserved areas. Patients reported considerable rates of mild or higher depression (54.3%) and anxiety (32.0%). Many utilized psychiatric (52.6%) or pain (20.6%) medications, while engagement in psychotherapy was low (5.1%). Patients reported impacts on quality of life, fatigue, and health-related quality of life, and the most common Top Problems were: "Shortness of breath, Breathlessness, Getting winded," "Fatigue/Low energy," and "Cough/Choking."
Conclusion: A licensed psychologist was successfully integrated into the NTM program. The disparity between PRO results and psychotherapy engagement highlights a key opportunity for mental health interventions. Integrated psychological services may provide streamlined access to mental healthcare.