John Mac
Senior Member (Voting Rights)
n=31
Improvement of immune dysregulation in individuals with long COVID at 24-months following SARS-CoV-2 infection
Abstract
This study investigates the humoral and cellular immune responses and health-related quality of life measures in individuals with mild to moderate long COVID (LC) compared to age and gender matched recovered COVID-19 controls (MC) over 24 months.
LC participants show elevated nucleocapsid IgG levels at 3 months, and higher neutralizing capacity up to 8 months post-infection. Increased spike-specific and nucleocapsid-specific CD4+ T cells, PD-1, and TIM-3 expression on CD4+ and CD8+ T cells were observed at 3 and 8 months, but these differences do not persist at 24 months.
Some LC participants had detectable IFN-γ and IFN-β, that was attributed to reinfection and antigen re-exposure. Single-cell RNA sequencing at the 24 month timepoint shows similar immune cell proportions and reconstitution of naïve T and B cell subsets in LC and MC.
No significant differences in exhaustion scores or antigen-specific T cell clones are observed. These findings suggest resolution of immune activation in LC and return to comparable immune responses between LC and MC over time.
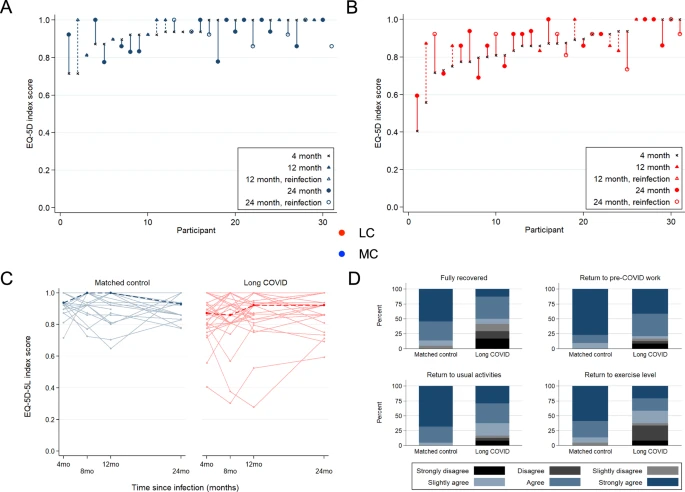
Improvement in self-reported health-related quality of life at 24 months was also evident in the majority of LC (62%). PTX3, CRP levels and platelet count are associated with improvements in health-related quality of life.
https://www.nature.com/articles/s41467-024-47720-8
Improvement of immune dysregulation in individuals with long COVID at 24-months following SARS-CoV-2 infection
Abstract
This study investigates the humoral and cellular immune responses and health-related quality of life measures in individuals with mild to moderate long COVID (LC) compared to age and gender matched recovered COVID-19 controls (MC) over 24 months.
LC participants show elevated nucleocapsid IgG levels at 3 months, and higher neutralizing capacity up to 8 months post-infection. Increased spike-specific and nucleocapsid-specific CD4+ T cells, PD-1, and TIM-3 expression on CD4+ and CD8+ T cells were observed at 3 and 8 months, but these differences do not persist at 24 months.
Some LC participants had detectable IFN-γ and IFN-β, that was attributed to reinfection and antigen re-exposure. Single-cell RNA sequencing at the 24 month timepoint shows similar immune cell proportions and reconstitution of naïve T and B cell subsets in LC and MC.
No significant differences in exhaustion scores or antigen-specific T cell clones are observed. These findings suggest resolution of immune activation in LC and return to comparable immune responses between LC and MC over time.
Improvement in self-reported health-related quality of life at 24 months was also evident in the majority of LC (62%). PTX3, CRP levels and platelet count are associated with improvements in health-related quality of life.
https://www.nature.com/articles/s41467-024-47720-8