Actually, just reading that last comment of mine, what this study shows is that the whole package of those alternative therapies are not worth anything much. And therefore, neither are the individual therapies. If mindfulness or acupressure or naturopathy and whatever else the clinic has been offering made any significant difference, this clinic would not be finding that people reported no significant changes in symptoms.
In fact, it's quite possible that there is some harm being done, which is not being measured, because people who think they are being harmed by a clinic don't tend to stick around to fill out surveys at discharge.
Of course it could be argued that this poor result proves that pacing doesn't help either. I'd argue that
1. This clinic does not seem to be offering very good advice, even on pacing, making it overly complicated and essentially pacing up, and
2. Probably most of the people attending the clinic had already worked out much of their pacing strategy before they came to the clinic. It comes naturally - you do stuff, you get clobbered by PEM, eventually you learn to do a bit less and do it a bit differently, and
So, it is evidence that providing (poor) advice on pacing at the time when people eventually get to a specialist clinic is not helpful, but it is not evidence that an adaption to the constraints imposed by ME/CFS is not helpful.
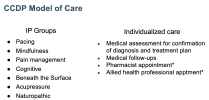
I think this paper is incredibly important. It is essentially the result of a long experiment. It blows the whole idea of a 'multi-disciplinary clinic' out of the water. The package this clinic offered is similar to what is promoted by Peter Gladwell and what the MEA seems to be totally on board with.
@Russell Fleming,
@sarahtyson - you need to look carefully at the paper. AfME too, and the people working on the new Australian guideline
@Simone. Specialist clinics where all sorts of woo is allowed to run free and that don't have a really clear focus on research are a waste of everyone's time, funds, hope and effort.
If Luis Nacul does genuinely care about people with ME/CFS, he will now make it abundantly clear around the world that this model does not work, and that it slows progress towards a better understanding of the illness. I don't know if anyone here knows him? If so, perhaps he could be encouraged to now make a positive difference? He is in a unique position to do so.