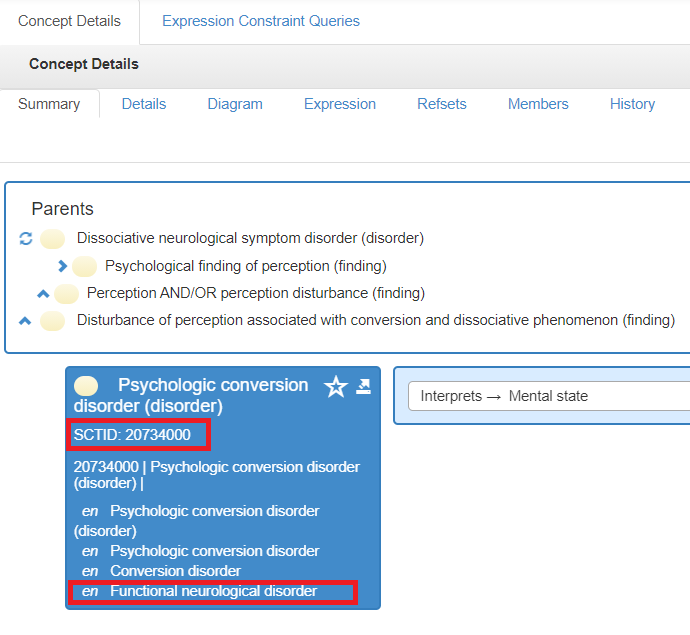
Functional Neurological Disorder at University Hospitals Plymouth NHS Trust
This webpage provides information for people with Functional Neurological Disorder and its symptoms, their carers
and their health professionals. We hope that you find it useful but please do let us know if there is anything else you
would like information about.
What is FND?
To help you understand the condition, we are going to break down its name:
FUNCTION: is how your body works
NEUROLOGICAL: is anything to do with your nerves and the messages they send to our brains
DISORDER: is when something doesn’t work as well as it should
So, to put it together, FND is a condition that affects your brain and causes your body not to function as it should.
Your brain receives millions of messages from the nerves around your body every single second. Sometimes our
brains can’t cope as well as it should with all of these messages, and we can start to experience neurological
symptoms. This is what FND is.
It is important to know that FND is not due to any brain damage or disease of your nervous system. FND is not
dangerous in itself, but people can injure themselves as a result of their symptoms. FND does not cause any damage
inside your brain or body.
FND can affect anyone. It often happens to people who are good at ‘putting up’ with difficult situations or stressful
events and can ‘carry on’ under pressure for a long time.
The exact prevalence of those diagnosed with FND is unknown however we know that FND does not discriminate. At
Derriford Hospital, FND symptoms are amongst the most common reasons why someone may be a Neurologist.
Symptoms
The symptoms that you may be experiencing are called Functional Neurological Symptoms (FNS). They are real and
genuine and can be debilitating to those experiencing them.
The most common symptoms are:
- Motor Dysfunction
- Functional limb weakness / paralysis
- Functional movement disorders including tremor, spasms (dystonia), jerky movements (myoclonus) and problems with walking (gait disorder)
- Functional speech symptoms including whispering speech (dysphonia) and slurred or stuttering speech
- Sensory Dysfunction
- Functional sensory disturbance includes altered sensation e.g. numbness, tingling or pain in the face, torso or limbs. This often occurs on one side of the body
- Functional visual symptoms including loss of vision or double vision
- Episodes of Altered Awareness
- Dissociative (non-epileptic) seizures, blackouts and faints. These symptoms can overlap and can look like epileptic seizures or faints (syncope).
Other physical and psychological symptoms are commonly experienced by patients with FND but may not be
present. These include:
- Chronic pains
- Bowel and bladder symptoms
- Fatigue
- Anxiety
- Memory symptoms
- Sleep problems
- Depression
Referral and Diagnosis Process
FND symptoms are often thought to be something else at first, but a Neurologist or Neuropsychologist knows the
important differences to look for to make the FND diagnosis.
If you feel you, or someone that you know, may be experiencing symptoms of FND, you should get an appointment
to see your GP. If your GP agrees, you will be referred to a Neurologist.
It is important to know that although sometimes a diagnosis can be made quickly, it may be necessary to carry out
some tests that may take time.
People often feel uncomfortable or confused with the diagnosis of FND because they have not heard of it before or it
has taken a long time to get the diagnosis.
An FND diagnosis is made from positive signs and symptoms. It is not made because doctors cannot find another
diagnosis.
FND at Derriford Hospital
FND sits at the interface between Neurology and Psychology.
There is no medical treatment for FND because it is not caused by disease or damage to the nervous system.
Research suggests that people who experience FND can benefit from psychological or physical therapy to help with
their symptoms, in the right circumstances.
Once referred by your GP, you will see one of our Neurologists and Neuropsychologists in our joint FNS clinic.
Treatment is currently made up on three stages:
- Information: Learning about what FND is and how it happens
- Stabilising: Strategies to control symptoms and reduce episodes
- Support making changes: Find new ways to manage stressful situations and patterns of coping that prevent FND returning in future – usually with an outpatient psychological therapist.