Simon M
Senior Member (Voting Rights)
Where is missing data missing from, and why?
The paper often says that the lack of concordance between cohorts is often due to missing data, but it isn't clear how this happens.
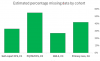
Much of this is simply because the four cohorts are defined by four UKB data fields, and a small majority of people have no data in those fields:

Data not missing at random
This missing hospital recoreds appear to be missing at random, at least as far as CFS status. However, pain questionnaire data is not missing at random: 41% of those who reported CFS at baseline assessment have PQ data, compared with 33% for all the UKB. People with health problems are more likely to complete a voluntary questionnaire about health issues than those without.
Summary: All UKB participants have baseline assessment data (with self-reported serious illnesses), and almost all have hospital records (with diagnosis codes). Nearly half have GP records (with diagnosis codes), and a third completed the Pain questionnaire, which asks about diagnoses of specific illnesses.
The paper often says that the lack of concordance between cohorts is often due to missing data, but it isn't clear how this happens.
Much of this is simply because the four cohorts are defined by four UKB data fields, and a small majority of people have no data in those fields:

- Every UKB participant was asked if they had a serious illness or disability diagnosed by a doctor at the initial assessment, and asked what that was, so there is no missing data here. (c1)
- Every participant gave consent to share medical records. UKB has hospital data for 89%. (C3)
- However, UKB only has primary care data for 46% due to problems accessing data. (C4)
- And only 33% completed the Pain Questionnaire. (C2)
Data not missing at random
This missing hospital recoreds appear to be missing at random, at least as far as CFS status. However, pain questionnaire data is not missing at random: 41% of those who reported CFS at baseline assessment have PQ data, compared with 33% for all the UKB. People with health problems are more likely to complete a voluntary questionnaire about health issues than those without.
Attachments
Last edited: