Deep abdominal breathing reduces heart rate and symptoms during orthostatic challenge in patients with postural orthostatic tachycardia syndrome
Background and purpose: This study investigated the effects of deep abdominal breathing on cardiovascular parameters and symptoms in patients with postural orthostatic tachycardia syndrome (POTS) during head-up tilt-table (HUT) challenge.Methods: Thirty POTS patients completed two consecutive rounds of 10-min HUT in a crossover design. One round was HUT without intervention, and one round combined the HUT with deep breathing at a rate of 6 breaths/min. Cardiovascular parameters, including mean blood pressure and maximum and mean heart rate (HR), were measured supine and standing. Symptoms were assessed using the Vanderbilt Orthostatic Symptom Score (VOSS).
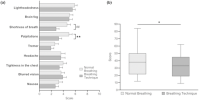
Results: During the breathing technique, the mean HR increase was -7.35 bpm (95% confidence interval [CI] = -11.71 to -2.98), and the maximum HR increase was -6.27 bpm (95% CI = -11.85 to -0.68, p = 0.041), significantly lower compared to normal breathing. Additionally, improvements were observed in all absolute cardiovascular parameters during standing, with VOSS symptoms simultaneously and significantly decreasing by -5.38 (95% CI = -10.43 to -0.36).
Conclusions: Slow deep abdominal breathing can act as a simple technique to reduce the standing HR increase upon HUT in patients with POTS. This suggests that modulation of the cardiopulmonary neurocircuits and the respiratory pump may reduce HR increase and symptoms in patients with POTS. The findings of this study highlight the use of a safe, zero-cost, and simple behavioral tool to suggest to POTS patients for symptom relief apart from standard treatment. The observed improvements in cardiovascular parameters and symptoms offer a promising therapeutic approach for patients in times of inadequate treatment options.