Covid-19 vaccine effectiveness against post-covid-19 condition among 589 722 individuals in Sweden: population based cohort study
Lisa Lundberg-Morris; Susannah Leach; Yiyi Xu; Jari Martikainen; Ailiana Santosa; Magnus Gisslén; Huiqi Li; Fredrik Nyberg; Maria Bygdell
Objectives
To investigate the effectiveness of primary covid-19 vaccination (first two doses and first booster dose within the recommended schedule) against post-covid-19 condition (PCC).
Design
Population based cohort study.
Setting
Swedish Covid-19 Investigation for Future Insights—a Population Epidemiology Approach using Register Linkage (SCIFI-PEARL) project, a register based cohort study in Sweden.
Participants
All adults (≥18 years) with covid-19 first registered between 27 December 2020 and 9 February 2022 (n=589 722) in the two largest regions of Sweden. Individuals were followed from a first infection until death, emigration, vaccination, reinfection, a PCC diagnosis (ICD-10 diagnosis code U09.9), or end of follow-up (30 November 2022), whichever came first. Individuals who had received at least one dose of a covid-19 vaccine before infection were considered vaccinated.
Main outcome measure
The primary outcome was a clinical diagnosis of PCC. Vaccine effectiveness against PCC was estimated using Cox regressions adjusted for age, sex, comorbidities (diabetes and cardiovascular, respiratory, and psychiatric disease), number of healthcare contacts during 2019, socioeconomic factors, and dominant virus variant at time of infection.
Results
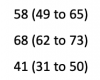
Of 299 692 vaccinated individuals with covid-19, 1201 (0.4%) had a diagnosis of PCC during follow-up, compared with 4118 (1.4%) of 290 030 unvaccinated individuals. Covid-19 vaccination with any number of doses before infection was associated with a reduced risk of PCC (adjusted hazard ratio 0.42, 95% confidence interval 0.38 to 0.46), with a vaccine effectiveness of 58%. Of the vaccinated individuals, 21 111 received one dose only, 205 650 received two doses, and 72 931 received three or more doses. Vaccine effectiveness against PCC for one dose, two doses, and three or more doses was 21%, 59%, and 73%, respectively.
Conclusions
The results of this study suggest a strong association between covid-19 vaccination before infection and reduced risk of receiving a diagnosis of PCC. The findings highlight the importance of primary vaccination against covid-19 to reduce the population burden of PCC.
Link | PDF (BMJ)
Lisa Lundberg-Morris; Susannah Leach; Yiyi Xu; Jari Martikainen; Ailiana Santosa; Magnus Gisslén; Huiqi Li; Fredrik Nyberg; Maria Bygdell
Objectives
To investigate the effectiveness of primary covid-19 vaccination (first two doses and first booster dose within the recommended schedule) against post-covid-19 condition (PCC).
Design
Population based cohort study.
Setting
Swedish Covid-19 Investigation for Future Insights—a Population Epidemiology Approach using Register Linkage (SCIFI-PEARL) project, a register based cohort study in Sweden.
Participants
All adults (≥18 years) with covid-19 first registered between 27 December 2020 and 9 February 2022 (n=589 722) in the two largest regions of Sweden. Individuals were followed from a first infection until death, emigration, vaccination, reinfection, a PCC diagnosis (ICD-10 diagnosis code U09.9), or end of follow-up (30 November 2022), whichever came first. Individuals who had received at least one dose of a covid-19 vaccine before infection were considered vaccinated.
Main outcome measure
The primary outcome was a clinical diagnosis of PCC. Vaccine effectiveness against PCC was estimated using Cox regressions adjusted for age, sex, comorbidities (diabetes and cardiovascular, respiratory, and psychiatric disease), number of healthcare contacts during 2019, socioeconomic factors, and dominant virus variant at time of infection.
Results
Of 299 692 vaccinated individuals with covid-19, 1201 (0.4%) had a diagnosis of PCC during follow-up, compared with 4118 (1.4%) of 290 030 unvaccinated individuals. Covid-19 vaccination with any number of doses before infection was associated with a reduced risk of PCC (adjusted hazard ratio 0.42, 95% confidence interval 0.38 to 0.46), with a vaccine effectiveness of 58%. Of the vaccinated individuals, 21 111 received one dose only, 205 650 received two doses, and 72 931 received three or more doses. Vaccine effectiveness against PCC for one dose, two doses, and three or more doses was 21%, 59%, and 73%, respectively.
Conclusions
The results of this study suggest a strong association between covid-19 vaccination before infection and reduced risk of receiving a diagnosis of PCC. The findings highlight the importance of primary vaccination against covid-19 to reduce the population burden of PCC.
Link | PDF (BMJ)