Seems like the literature is confusing here. Consensus seems to be that no antivirals (AV) are effective against EBV.
 pmc.ncbi.nlm.nih.gov
pmc.ncbi.nlm.nih.gov
But then there are case studies showing certain AVs are effective.
 www.frontiersin.org
www.frontiersin.org

 www.cureus.com
www.cureus.com
More recently, evidence is presented that that tenofovir prodrugs tenofovir disoproxil fumarate (TDF) and tenofovir alafenamide (TAF), are highly effective against EBV (in vitro)

 pubmed.ncbi.nlm.nih.gov
pubmed.ncbi.nlm.nih.gov
In vivo
Trial
Does anyone have any idea on the current thinking/consensus (if any) on this topic?
Novel Therapeutics for Epstein–Barr Virus - PMC
Epstein–Barr virus (EBV) is a human γ-herpesvirus that infects up to 95% of the adult population. Primary EBV infection usually occurs during childhood and is generally asymptomatic, though the virus can cause infectious mononucleosis in 35–50% of ...
But then there are case studies showing certain AVs are effective.
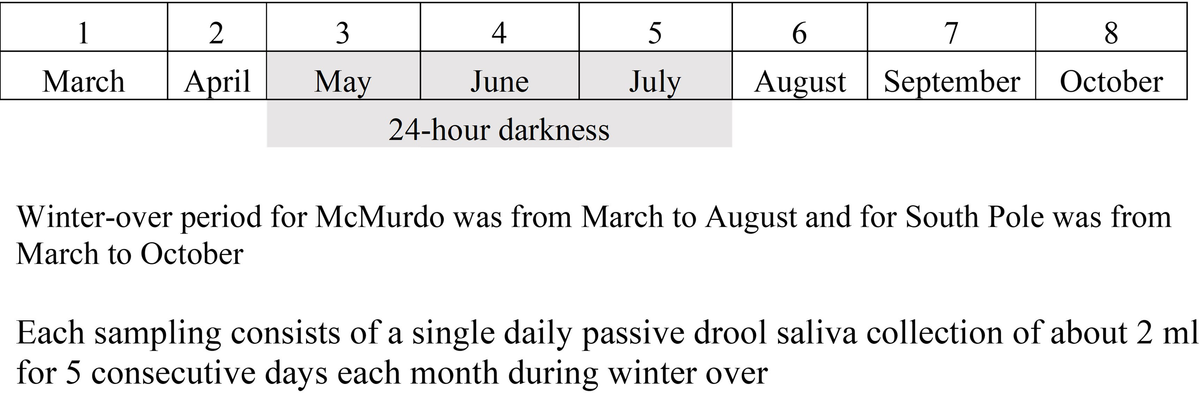
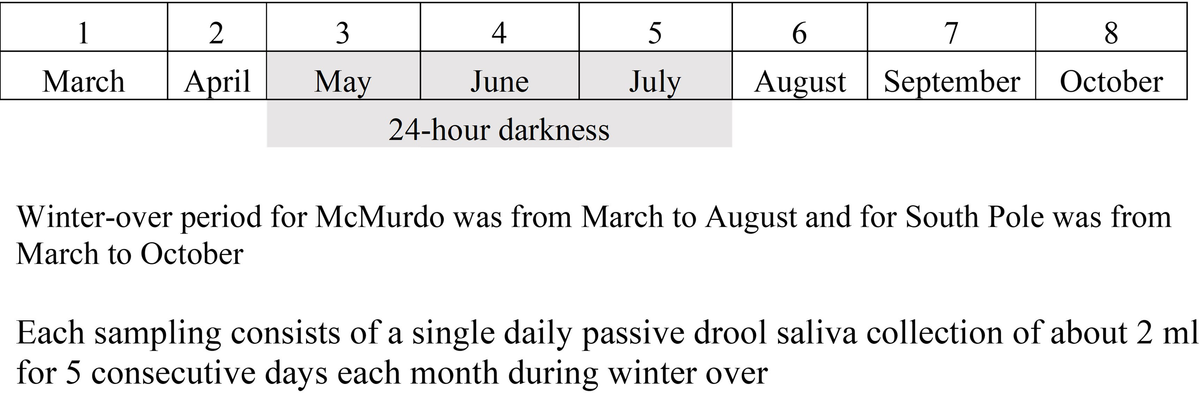
Frontiers | Antiviral treatment with valacyclovir reduces virus shedding in saliva of Antarctic expeditioners
Reactivation of herpes viruses such as Epstein-Barr virus (EBV), herpes simplex virus 1 (HSV1), and varicella zoster virus (VZV) increase in astronauts durin...

Acyclovir as a Novel Treatment for Severe Chronic Active Epstein-Barr Virus
Epstein-Barr virus (EBV) is a widely infectious pathogen affecting most of the global population at some point in their life. While, typically, primary infections are subclinical, chronic persistence of the virus due to T-cell proliferation can cause severe complications. Acute hepatitis due to...
More recently, evidence is presented that that tenofovir prodrugs tenofovir disoproxil fumarate (TDF) and tenofovir alafenamide (TAF), are highly effective against EBV (in vitro)

Tenofovir prodrugs potently inhibit Epstein-Barr virus lytic DNA replication by targeting the viral DNA polymerase - PubMed
Epstein-Barr virus (EBV) is a ubiquitous human γ-herpesvirus that establishes life-long infection and increases the risk for the development of several cancers and autoimmune diseases. The mechanisms by which chronic EBV infection leads to subsequent disease remain incompletely understood. Lytic...
In vivo
Trial
Effects of Antiviral Therapies on Epstein-Barr Virus Replication
This research study is being performed to find out if Truvada (tenofovir/emtricitabine), an antiviral drug with activity against the Epstein Barr virus (EBV), can reduce EBV levels in saliva and blood in people with multiple sclerosis (MS). A second goal is to find out if Truvada (tenofovir/...
ctv.veeva.com
Does anyone have any idea on the current thinking/consensus (if any) on this topic?
Last edited:
