Study 1
14 participants aged ≥ 55 years with no previous medical history of hypertension, cardiac disease, diabetes mellitus or epilepsy were enrolled on the study (see
Supplementary Table 1).
tVNS vs. sham effects on cardiac baroreflex and HRV
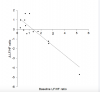
Change in baroreflex sensitivity (BRS) between baseline and tVNS significantly differed between the tVNS and sham visits (p = 0.028): there was a significantly greater increase in BRS during the tVNS visit (3.28 ± 0.59 ms/mmHg) compared to the sham visit (0.81 ± 0.68 ms/mmHg). Baseline heart rate variability (HRV), measured as ratio of LF/HF power, significantly predicted response to tVNS (R2 = 0.772, p < 0.001, see
Figure 1), where higher resting LF/HF ratio was associated with greater decreases during tVNS. Removing the potential outlier with a baseline LF/HF ratio > 5 had a slight impact on the regression (R2 = 0.480, p = 0.009). This HRV analysis revealed that the LF/HF ratio response of four participants was greater than a 20% increase, corresponding to a definition of responders previously applied [
11].