https://academic.oup.com/jcem/article/93/3/703/2598104?login=false
Attenuated Morning Salivary Cortisol Concentrations in a Population-Based Study of Persons with Chronic Fatigue Syndrome and Well Controls
Urs M. Nater, Elizabeth Maloney, Roumiana S. Boneva, Brian M. Gurbaxani, Jin-Mann Lin, James F. Jones, William C. Reeves, Christine Heim
Abstract
Context: A substantial body of research on the pathophysiology of chronic fatigue syndrome (CFS) has focused on hypothalamic-pituitary-adrenal axis dysregulation. The cortisol awakening response has received particular attention as a marker of hypothalamic-pituitary-adrenal axis dysregulation.
Objective: The objective of the current study was to evaluate morning salivary cortisol profiles in persons with CFS and well controls identified from the general population.
Design and Setting: We conducted a case-control study at an outpatient research clinic.
Cases and Other Participants: We screened a sample of 19,381 residents of Georgia and identified those with CFS and a matched sample of well controls. Seventy-five medication-free CFS cases and 110 medication-free well controls provided complete sets of saliva samples.
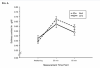
Main Outcome Measures: We assessed free cortisol concentrations in saliva collected on a regular workday immediately upon awakening and 30 and 60 min after awakening.
Results: There was a significant interaction effect, indicating different profiles of cortisol concentrations over time between groups, with the CFS group showing an attenuated morning cortisol profile. Notably, we observed a sex difference in this effect. Women with CFS exhibited significantly attenuated morning cortisol profiles compared with well women. In contrast, cortisol profiles were similar in men with CFS and male controls.
Conclusions: CFS was associated with an attenuated morning cortisol response, but the effect was limited to women. Our results suggest that a sex difference in hypocortisolism may contribute to increased risk of CFS in women.
Attenuated Morning Salivary Cortisol Concentrations in a Population-Based Study of Persons with Chronic Fatigue Syndrome and Well Controls
Urs M. Nater, Elizabeth Maloney, Roumiana S. Boneva, Brian M. Gurbaxani, Jin-Mann Lin, James F. Jones, William C. Reeves, Christine Heim
Abstract
Context: A substantial body of research on the pathophysiology of chronic fatigue syndrome (CFS) has focused on hypothalamic-pituitary-adrenal axis dysregulation. The cortisol awakening response has received particular attention as a marker of hypothalamic-pituitary-adrenal axis dysregulation.
Objective: The objective of the current study was to evaluate morning salivary cortisol profiles in persons with CFS and well controls identified from the general population.
Design and Setting: We conducted a case-control study at an outpatient research clinic.
Cases and Other Participants: We screened a sample of 19,381 residents of Georgia and identified those with CFS and a matched sample of well controls. Seventy-five medication-free CFS cases and 110 medication-free well controls provided complete sets of saliva samples.
Main Outcome Measures: We assessed free cortisol concentrations in saliva collected on a regular workday immediately upon awakening and 30 and 60 min after awakening.
Results: There was a significant interaction effect, indicating different profiles of cortisol concentrations over time between groups, with the CFS group showing an attenuated morning cortisol profile. Notably, we observed a sex difference in this effect. Women with CFS exhibited significantly attenuated morning cortisol profiles compared with well women. In contrast, cortisol profiles were similar in men with CFS and male controls.
Conclusions: CFS was associated with an attenuated morning cortisol response, but the effect was limited to women. Our results suggest that a sex difference in hypocortisolism may contribute to increased risk of CFS in women.