Individualised aerobic and resistance exercise training improves exercise tolerance in individuals with Long COVID: findings from the PERCEIVE randomised controlled trial
E Howden, L Burnham, J Smith, K Whitmore, K Morrison, R Hoare, Y Sata, Q Huynh, T Marwick
[Line breaks added]
Background
"Long COVID" is reported to occur in about 10% of people after COVID-19 infection, with predominant symptoms of exercise intolerance and fatigue. Exercise training is an effective treatment for these symptoms in other settings, but may have adverse sequelae in chronic fatigue syndrome, which overlaps with Long COVID. The efficacy of training in Long COVID is unknown.
Purpose
To evaluate the effect of a multidisciplinary exercise intervention (MExT) including medical management of left ventricular (LV) dysfunction and a 6-month personalized supervised aerobic and resistance exercise training program in an randomised control trial (RCT) comparison with usual care (UC) in people with long COVID.
Method
In this multicenter, two-arm, parallel, RCT we enrolled adults who were experiencing ongoing symptoms (>12 weeks) and a reduced VO2 peak (< age-sex-predicted) following acute COVID-19. Participants were randomised (stratified by age [40-64; >65] and hospitalization status) to MExT (personalised exercise training + medical management of LV dysfunction and CV risk factors) vs UC for 6-months, with baseline and follow-up cardiopulmonary exercise testing (CPET). The primary outcome was change in peak oxygen uptake (VO2peak). Secondary outcomes included change in quality of life (AQoL-8D) and mood (PHQ-9). Exercise prescription and adherence were monitored via heart monitors.
Results
In total 133 participants (mean age, 53±9 years; 87 females (65%) and 46 males (35%)) were randomised 1:1 to MExT (n=66) or UC (67) between October 2022 – May 2024, 11 [5-29] months post-acute infection and 57 MExT and 60 UC participants completed follow-up testing. The MExT group completed a median of 53 aerobic (range 2-225) and median of 68 resistance (range 1-68 sessions) exercise sessions over the 6-month period and received CV risk factor optimization (50%) or initiation of cardioprotective therapy (27%).
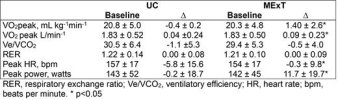
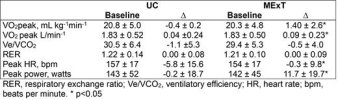
The CPETs results are summarised in the table. At 6 months, there were between group differences in indexed VO2 peak of 1.74 mL kg-1 min-1(95% confidence interval (CI): 0.71, 2.76) p= 0.001), absolute VO2 of 0.14 L.min-1(95% CI: 0.05, 0.22; p value =0.003) and peak watts of 11.5w (95%CI: 4.3, 18.7, p=0.002).
Other CPET parameters were not statistically different at 6-months (Ve/VCO2 slope, RER), except for peak HR which was ~6 beats lower in UC.
There was no significant effect of the intervention on mood (PHQ-9 between group difference 0.60 (-0.82, 2.02; p = 0.40) or quality of life (AQoL-8D score 0.01(-0.04, 0.06; p =0.72).
Conclusion
These results suggest that a carefully supervised and individualised exercise program improves cardiorespiratory fitness in individuals with long COVID.
Web | PDF | European Heart Journal | Abstract only
E Howden, L Burnham, J Smith, K Whitmore, K Morrison, R Hoare, Y Sata, Q Huynh, T Marwick
[Line breaks added]
Background
"Long COVID" is reported to occur in about 10% of people after COVID-19 infection, with predominant symptoms of exercise intolerance and fatigue. Exercise training is an effective treatment for these symptoms in other settings, but may have adverse sequelae in chronic fatigue syndrome, which overlaps with Long COVID. The efficacy of training in Long COVID is unknown.
Purpose
To evaluate the effect of a multidisciplinary exercise intervention (MExT) including medical management of left ventricular (LV) dysfunction and a 6-month personalized supervised aerobic and resistance exercise training program in an randomised control trial (RCT) comparison with usual care (UC) in people with long COVID.
Method
In this multicenter, two-arm, parallel, RCT we enrolled adults who were experiencing ongoing symptoms (>12 weeks) and a reduced VO2 peak (< age-sex-predicted) following acute COVID-19. Participants were randomised (stratified by age [40-64; >65] and hospitalization status) to MExT (personalised exercise training + medical management of LV dysfunction and CV risk factors) vs UC for 6-months, with baseline and follow-up cardiopulmonary exercise testing (CPET). The primary outcome was change in peak oxygen uptake (VO2peak). Secondary outcomes included change in quality of life (AQoL-8D) and mood (PHQ-9). Exercise prescription and adherence were monitored via heart monitors.
Results
In total 133 participants (mean age, 53±9 years; 87 females (65%) and 46 males (35%)) were randomised 1:1 to MExT (n=66) or UC (67) between October 2022 – May 2024, 11 [5-29] months post-acute infection and 57 MExT and 60 UC participants completed follow-up testing. The MExT group completed a median of 53 aerobic (range 2-225) and median of 68 resistance (range 1-68 sessions) exercise sessions over the 6-month period and received CV risk factor optimization (50%) or initiation of cardioprotective therapy (27%).
The CPETs results are summarised in the table. At 6 months, there were between group differences in indexed VO2 peak of 1.74 mL kg-1 min-1(95% confidence interval (CI): 0.71, 2.76) p= 0.001), absolute VO2 of 0.14 L.min-1(95% CI: 0.05, 0.22; p value =0.003) and peak watts of 11.5w (95%CI: 4.3, 18.7, p=0.002).
Other CPET parameters were not statistically different at 6-months (Ve/VCO2 slope, RER), except for peak HR which was ~6 beats lower in UC.
There was no significant effect of the intervention on mood (PHQ-9 between group difference 0.60 (-0.82, 2.02; p = 0.40) or quality of life (AQoL-8D score 0.01(-0.04, 0.06; p =0.72).
Conclusion
These results suggest that a carefully supervised and individualised exercise program improves cardiorespiratory fitness in individuals with long COVID.
Web | PDF | European Heart Journal | Abstract only
