You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
A thread to share your experiences of orthostatic intolerance - problems being upright.
- Thread starter Trish
- Start date
ahimsa
Senior Member (Voting Rights)
Finally responding to this, hope it helps and is not too late.
Symptoms:
My main orthostatic intolerance (OI) symptoms are nausea, increased heart rate, feeling lightheaded, feeling short of breath, not being able to think very well, not being able to talk much. I tell people I need to sit down before I can think. I tell my husband that he needs to wait until I'm sitting down to ask me a question. Even if it's something quite simple I often can't think and can't answer while I'm standing. I sometimes get a cold sweat or clammy feeling.
If I'm standing then I quickly feel a strong urge to *sit down now*. Putting my feet up helps even more - sitting on the couch with my legs crossed, lying in the recliner, or lying down flat (couch or bed).
I sometimes get the classic "coat hanger pain" between my shoulder blades. What helps relieve the pain for me is lying down with my feet higher than my head.
I often get chest pains. I think this is also a symptom of OI even though it doesn't often happen while I'm standing. It usually happens later on. Two reasons why I think chest pains are due to OI:
1) I got the same kind of chest pains on the tilt table test right before I fainted
2) several of the POTS documents mention chest pain as a symptom
My husband once commented on my "chair seeking" behavior as I go around the house on bad days. He said it's like someone swimming under the ice and looking for the next ice hole so they can come to the surface and take a breath. I thought that captured it pretty well. I can walk quickly from one place to the next (no problems with weakness) but I then I need to sit down.
Triggers:
As far as posture or position the worst symptoms come when I try to stand still, e.g., waiting in line at a store, trying to talk to someone while standing.
Next in line would be sitting upright at a desk with feet on the floor. For example, as a software engineer I used to sit still while coding for hours at a time. And then I wondered why I felt so bad the next day (I didn't realize it was a form of PEM). This may be a combination of mental fatigue and the muscle use (muscles used while sitting vs. reclining or lying flat). I'm not sure exactly how the OI interacts with PEM caused by mental/physical exertion.
At any rate, sitting upright in a chair with my feet on the ground will still cause symptoms for me eventuallly, it just happens more slowly than standing.
Heat is another big trigger. If it's too warm (that's over about 74 degrees F / 23 degrees C for me) my OI symptoms will come on more quickly.
If I've been resting a lot then my OI is not as bad. It takes longer to get to that "I have to sit down now" feeling.
But if I'm in PEM, or I've just been walking for a bit, then I feel more of that urge to sit down quickly.
Car seats can recline a bit so they are not as bad as straight backed chairs or benches. Benches without any back support are also more likely to cause symptoms than a chair with some angle and with back support. Some of this is an overlap between OI and just using muscles (exertion) so it's a bit hard to disentangle.
Having a full stomach (right after eating a full meal) makes symptoms worse. I need to rest for at least an hour after meals. If I want more energy so I can attend some event or finish some task I will skip eating. An empty stomach makes things easier.
Fainting:
I've only fainted 3 times. Two of those times happened during a tilt table test (1995 and 2003), just from standing, no isoproteronol was injected. I started getting symptoms at about 5 minutes but it took between 20 and 30 minutes before my blood pressure (BP) suddenly dropped to something very low (unmeasurable by the devices that were attached) I fainted.
After I fainted they put the table flat and gave me a saline IV to help me recover. My heart rate did increase some at the start but not enough for the diagnostic criteria for Postural Orthostatic Tachycardia Syndrome (POTS).
The diagnosis I got in 1995 was Neurally Mediated Hypotension (NMH). There have been a lot of changes since then and I don't know if the current diagnostic names are the same. But my understanding is that in spite of one the words being the same this diagnosis is different from the more typical Orthostatic Hypotension (OH) where the blood pressure drops within a few minutes of standing. If I'd had OH it would have been diagnosed more quickly since I never had any problem with the BP tests in the doctor's office where BP is taking while sitting then standing.
Many years later (not sure when, at least 5-6 years?) I did have an increase in heart rate on standing that met the POTS criteria. So my cardiologist said I had both NMH and POTS.
Things that help me:
I take midodrine, a prescription medicine, which is supposed to help keep the blood pressure from dropping.
I take salt tablets with meals every day. My diet wouldn't have much salt in it if it weren't for these salt tablets.
On an as needed basis I drink an electrolyte mix or ORS (oral rehydration solution). I use either unflavored pedialyte or something like Normalyte (a powder you mix with water). I feel better when I use an ORS that has some kind of sugar (e.g., glucose) although I have read other folks saying they don't notice any difference.
I avoid being in the heat. Our house and car have air conditioning for when it gets hot. Getting "pre-chilled" (being in the A/C and also drinking cold drinks) can help me to tolerate the heat (prevent the nausea and feeling dizzy or lightheaded) for a short time if needed.
I wear compression socks if it's not too hot. I think they help when I have to be upright for longer periods of time but I'm not 100% sure.
I rest in the recliner with my feet elevated.
I use a folding cane/seat for when I need to wait in line. It is not comfortable for more than 5-6 minutes (no back support) but it does help to be sitting instead of standing. So, it's not helpful for long lines but good for short lines.
I use a wheelchair in any situation with a long line (e.g., the airport).
Symptoms:
My main orthostatic intolerance (OI) symptoms are nausea, increased heart rate, feeling lightheaded, feeling short of breath, not being able to think very well, not being able to talk much. I tell people I need to sit down before I can think. I tell my husband that he needs to wait until I'm sitting down to ask me a question. Even if it's something quite simple I often can't think and can't answer while I'm standing. I sometimes get a cold sweat or clammy feeling.
If I'm standing then I quickly feel a strong urge to *sit down now*. Putting my feet up helps even more - sitting on the couch with my legs crossed, lying in the recliner, or lying down flat (couch or bed).
I sometimes get the classic "coat hanger pain" between my shoulder blades. What helps relieve the pain for me is lying down with my feet higher than my head.
I often get chest pains. I think this is also a symptom of OI even though it doesn't often happen while I'm standing. It usually happens later on. Two reasons why I think chest pains are due to OI:
1) I got the same kind of chest pains on the tilt table test right before I fainted
2) several of the POTS documents mention chest pain as a symptom
My husband once commented on my "chair seeking" behavior as I go around the house on bad days. He said it's like someone swimming under the ice and looking for the next ice hole so they can come to the surface and take a breath. I thought that captured it pretty well. I can walk quickly from one place to the next (no problems with weakness) but I then I need to sit down.
Triggers:
As far as posture or position the worst symptoms come when I try to stand still, e.g., waiting in line at a store, trying to talk to someone while standing.
Next in line would be sitting upright at a desk with feet on the floor. For example, as a software engineer I used to sit still while coding for hours at a time. And then I wondered why I felt so bad the next day (I didn't realize it was a form of PEM). This may be a combination of mental fatigue and the muscle use (muscles used while sitting vs. reclining or lying flat). I'm not sure exactly how the OI interacts with PEM caused by mental/physical exertion.
At any rate, sitting upright in a chair with my feet on the ground will still cause symptoms for me eventuallly, it just happens more slowly than standing.
Heat is another big trigger. If it's too warm (that's over about 74 degrees F / 23 degrees C for me) my OI symptoms will come on more quickly.
If I've been resting a lot then my OI is not as bad. It takes longer to get to that "I have to sit down now" feeling.
But if I'm in PEM, or I've just been walking for a bit, then I feel more of that urge to sit down quickly.
Car seats can recline a bit so they are not as bad as straight backed chairs or benches. Benches without any back support are also more likely to cause symptoms than a chair with some angle and with back support. Some of this is an overlap between OI and just using muscles (exertion) so it's a bit hard to disentangle.
Having a full stomach (right after eating a full meal) makes symptoms worse. I need to rest for at least an hour after meals. If I want more energy so I can attend some event or finish some task I will skip eating. An empty stomach makes things easier.
Fainting:
I've only fainted 3 times. Two of those times happened during a tilt table test (1995 and 2003), just from standing, no isoproteronol was injected. I started getting symptoms at about 5 minutes but it took between 20 and 30 minutes before my blood pressure (BP) suddenly dropped to something very low (unmeasurable by the devices that were attached) I fainted.
After I fainted they put the table flat and gave me a saline IV to help me recover. My heart rate did increase some at the start but not enough for the diagnostic criteria for Postural Orthostatic Tachycardia Syndrome (POTS).
The diagnosis I got in 1995 was Neurally Mediated Hypotension (NMH). There have been a lot of changes since then and I don't know if the current diagnostic names are the same. But my understanding is that in spite of one the words being the same this diagnosis is different from the more typical Orthostatic Hypotension (OH) where the blood pressure drops within a few minutes of standing. If I'd had OH it would have been diagnosed more quickly since I never had any problem with the BP tests in the doctor's office where BP is taking while sitting then standing.
Many years later (not sure when, at least 5-6 years?) I did have an increase in heart rate on standing that met the POTS criteria. So my cardiologist said I had both NMH and POTS.
Things that help me:
I take midodrine, a prescription medicine, which is supposed to help keep the blood pressure from dropping.
I take salt tablets with meals every day. My diet wouldn't have much salt in it if it weren't for these salt tablets.
On an as needed basis I drink an electrolyte mix or ORS (oral rehydration solution). I use either unflavored pedialyte or something like Normalyte (a powder you mix with water). I feel better when I use an ORS that has some kind of sugar (e.g., glucose) although I have read other folks saying they don't notice any difference.
I avoid being in the heat. Our house and car have air conditioning for when it gets hot. Getting "pre-chilled" (being in the A/C and also drinking cold drinks) can help me to tolerate the heat (prevent the nausea and feeling dizzy or lightheaded) for a short time if needed.
I wear compression socks if it's not too hot. I think they help when I have to be upright for longer periods of time but I'm not 100% sure.
I rest in the recliner with my feet elevated.
I use a folding cane/seat for when I need to wait in line. It is not comfortable for more than 5-6 minutes (no back support) but it does help to be sitting instead of standing. So, it's not helpful for long lines but good for short lines.
I use a wheelchair in any situation with a long line (e.g., the airport).
Last edited:
On an as needed basis I drink an electrolyte mix or ORS (oral rehydration solution). I use either unflavored pedialyte or something like Normalyte (a powder you mix with water). I feel better when I use an ORS that has some kind of sugar (e.g., glucose) although I have read other folks saying they don't notice any difference.
For the last month I have found ORS wonderful in reducing my calf cramp, dorsa flexion following an ankle injury 5 years ago and general widespread joint pain. The calf pain was diagnosed as over training syndrome but to me it felt like being held at the get-set moment permanently. I started with a daily sachet for a week but then reduced to half per day. Intentionally missing doses caused the symptoms to gradually return including the flexion. I certainly feel better and have slightly better sleep and energy.
wingate
Senior Member (Voting Rights)
Some personal observations about OI:
-It has worsened a lot over the course of my illness.
-The best way I can describe it is it feels like if I am standing, I am like a vessel for liquid, and there is a drain near my feet. The liquid is energy, and the longer I stand up, the more energy that drains out. That’s kind of physically how it feels, too.
-I often finding myself doing maneuvers to alleviate the OI- fidgeting or shifting my weight if I have to stand, also slouching is easier than standing up straight, crossing my legs(at the thigh and around the calf/ankle) when seated, with my knees or feet up on the couch back if lying down.
-Standing still is really bad. Or being seated with feet on the floor. Showering, etc.
-As my OI has worsened, I have noticed eating, particularly dinner, often triggers awful OI and I feel so weak after eating I can’t do much but lie down. I recently got a different watch, and the time between eating and bed is a highly stressful time (based on HR and HRV), even though I’m either lying down or sitting with legs up, so that seems to align with my symptoms.
I would be curious to know if others have any adaptations for eating and OI. I definitely opt for @ahimsa ’s strategic eating, but not eating enough causes its own set of symptoms.
-It has worsened a lot over the course of my illness.
-The best way I can describe it is it feels like if I am standing, I am like a vessel for liquid, and there is a drain near my feet. The liquid is energy, and the longer I stand up, the more energy that drains out. That’s kind of physically how it feels, too.
-I often finding myself doing maneuvers to alleviate the OI- fidgeting or shifting my weight if I have to stand, also slouching is easier than standing up straight, crossing my legs(at the thigh and around the calf/ankle) when seated, with my knees or feet up on the couch back if lying down.
-Standing still is really bad. Or being seated with feet on the floor. Showering, etc.
-As my OI has worsened, I have noticed eating, particularly dinner, often triggers awful OI and I feel so weak after eating I can’t do much but lie down. I recently got a different watch, and the time between eating and bed is a highly stressful time (based on HR and HRV), even though I’m either lying down or sitting with legs up, so that seems to align with my symptoms.
I would be curious to know if others have any adaptations for eating and OI. I definitely opt for @ahimsa ’s strategic eating, but not eating enough causes its own set of symptoms.
Im mostly disabled by my muscular pain/fatigue/weakness, sitting up hasn't caused big problems recently but standing is mostly difficult because of pain.
My OI is most noticable when I lay down, its like I can feel my blood go back up and fill up the inside of my skull. Sometimes I get a headache, usually just pressure building up. More of an overwhelmingly pleasant feeling, to the point of becoming unpleasant.
I have had 3 occasions where I fainted or was very close to fainting. Everytime, my hr was way lower then I expected. 2 times where during my sleep, with my hr dropping 20bpm lower compared to normal (its a 2 minute average, so most likely even lower), according to my watch, waking me up neaseated and generally out of it.
Both times I felt a need to stand up, but passed out when I came downstairs.
1 other time was very recent, when I had been sitting and active during dinner for a while. Felt neaseas, dizzy, according to my parents I visibly turned very pale, I felt like my heart rate was extremely high, but when I looked down onto my watch it was only at 60bpm (normally between 80-110 in such situation, 60 when asleep). I couldn't easily make the decision to lay down or do anything, but eventually did and symptoms quickly went away.
I am diagnosed with dysautonomia and POTS, and my blood pressure is overall low. Never had tilt table testing. I also take propranolol.
It is mostly just a more general difficulty to do things. My emotional regulation is worse, so is decision making. I often have to sit or lay down to make a decision or calm down from emotional stress. Often i feel out of breath, and I used to have bad headaches when upright (although they are treated well with propranolol, might have been migraines).
I can quickly warm something up, but bigger meals are done seated. Showering I do on the ground. I am also currently waiting on delivery of an active wheelchair with power assist, although as I said before my biggest problems are pain and fatigue, not the dysautonomia or OI.
My OI is most noticable when I lay down, its like I can feel my blood go back up and fill up the inside of my skull. Sometimes I get a headache, usually just pressure building up. More of an overwhelmingly pleasant feeling, to the point of becoming unpleasant.
I have had 3 occasions where I fainted or was very close to fainting. Everytime, my hr was way lower then I expected. 2 times where during my sleep, with my hr dropping 20bpm lower compared to normal (its a 2 minute average, so most likely even lower), according to my watch, waking me up neaseated and generally out of it.
Both times I felt a need to stand up, but passed out when I came downstairs.
1 other time was very recent, when I had been sitting and active during dinner for a while. Felt neaseas, dizzy, according to my parents I visibly turned very pale, I felt like my heart rate was extremely high, but when I looked down onto my watch it was only at 60bpm (normally between 80-110 in such situation, 60 when asleep). I couldn't easily make the decision to lay down or do anything, but eventually did and symptoms quickly went away.
I am diagnosed with dysautonomia and POTS, and my blood pressure is overall low. Never had tilt table testing. I also take propranolol.
It is mostly just a more general difficulty to do things. My emotional regulation is worse, so is decision making. I often have to sit or lay down to make a decision or calm down from emotional stress. Often i feel out of breath, and I used to have bad headaches when upright (although they are treated well with propranolol, might have been migraines).
I can quickly warm something up, but bigger meals are done seated. Showering I do on the ground. I am also currently waiting on delivery of an active wheelchair with power assist, although as I said before my biggest problems are pain and fatigue, not the dysautonomia or OI.
AliceLily
Senior Member (Voting Rights)
I will have to check whether I have already post in this thread but just while I remember a few things I found it really hard for years to move my head quick enough to cross a road. It felt like my head was filled with fluid and turning my head from side to side made me off balance and my gait would try to steady myself.
I also went through a period at very severe ME where my neck and spine felt like jelly. I caught hardly hold my head up or sit upright.
Standing still was awful, like others have said I felt like I had to try to move so I wouldn't faint/collapse. Another thing I remember vividly is the amount of focus and concentration that was needed. All my focus was so concentrated on either trying to stay upright, trying to walk straight as possible etc.
I also went through a period at very severe ME where my neck and spine felt like jelly. I caught hardly hold my head up or sit upright.
Standing still was awful, like others have said I felt like I had to try to move so I wouldn't faint/collapse. Another thing I remember vividly is the amount of focus and concentration that was needed. All my focus was so concentrated on either trying to stay upright, trying to walk straight as possible etc.
ChronicallyOverIt
Senior Member (Voting Rights)
My Orthostatic intolerance came on quite suddenly when I was already 3 years into CFS. Maybe I had a minor version before but never noticed.
I stupidly was very mild at the time and decided to go mountain biking with some old friends, this was a huge huge step up in my activity, but at the time I had been pushing and crashing and accepting it. I biked for 3-4hrs, after biking my heart rate would not come down out of the 110-120bpm range. I even slept that night with my apple watch on and it tracked my heart rate in 90-110bpm range while sleeping. The following day I noticed I almost fainted when getting up from bed. My hear rate eventually went down into the 60-70s the day.
After this showers standing up would trigger my BPM to the 140bpm range. Standing to using bathroom would spike my BPM in the 110bpm-120bpm and stay there, where my resting sitting is in the 60s BPM. This is when I put two and two together. Did NASA lean my BPM went from 65bpm to 110-120bpm and stays there, sometimes rising if I am feeling bad that day over ten minutes. Went to my GP did ECG and holter but found nothing wrong. That's when I started learning about POT(s).
Simple tasks became hard overnight, suddenly walking to the grocery store, lifting anything, or any activity would cause me to sweat. Before I would barley sweat, I could get away without laundering a shirt for a day or two. Now my shirts are done and dusted at end of day I sweat so much.
Again standing still is worst, legs walking pumps blood I think so its better. Mestinon has been a life saver and has allowed me to shower sitting down again in the 100bpm range, along with improve my QoL over all.
I stupidly was very mild at the time and decided to go mountain biking with some old friends, this was a huge huge step up in my activity, but at the time I had been pushing and crashing and accepting it. I biked for 3-4hrs, after biking my heart rate would not come down out of the 110-120bpm range. I even slept that night with my apple watch on and it tracked my heart rate in 90-110bpm range while sleeping. The following day I noticed I almost fainted when getting up from bed. My hear rate eventually went down into the 60-70s the day.
After this showers standing up would trigger my BPM to the 140bpm range. Standing to using bathroom would spike my BPM in the 110bpm-120bpm and stay there, where my resting sitting is in the 60s BPM. This is when I put two and two together. Did NASA lean my BPM went from 65bpm to 110-120bpm and stays there, sometimes rising if I am feeling bad that day over ten minutes. Went to my GP did ECG and holter but found nothing wrong. That's when I started learning about POT(s).
Simple tasks became hard overnight, suddenly walking to the grocery store, lifting anything, or any activity would cause me to sweat. Before I would barley sweat, I could get away without laundering a shirt for a day or two. Now my shirts are done and dusted at end of day I sweat so much.
Again standing still is worst, legs walking pumps blood I think so its better. Mestinon has been a life saver and has allowed me to shower sitting down again in the 100bpm range, along with improve my QoL over all.
boolybooly
Senior Member (Voting Rights)
OI manifests when I stand from bending down or crouching for a short while, I feel dizzy and know I can faint, the blood supply to my head fails and I have to bend over to make it easier for the blood to reach my head. If I slowly straighten up then adaptation occurs over twenty seconds or so and I am no longer in danger of blacking out.
This is not helped by heart arrhythmia, which is variable but has become worse since contracting an infection, suspected covid variant, in the last half of 2025. Unfortunately I have an immune dysfunction which means viruses can recur and often do as has this one. Myocarditis is an accepted symptom of covid and my guess is this is what is causing the tendency to skipped beats. When my heartbeat rate is trying to increase it is plagued by premature beats every other beat and so skips alternate beats resulting in a pulse rate half of normal, eg after mild exertion a pulse of 40/min, when it is trying to make 80. This does not help getting blood to my head when OI is in effect due to changing body orientation and heart to head angle changes from horizontal to vertical.
This is not helped by heart arrhythmia, which is variable but has become worse since contracting an infection, suspected covid variant, in the last half of 2025. Unfortunately I have an immune dysfunction which means viruses can recur and often do as has this one. Myocarditis is an accepted symptom of covid and my guess is this is what is causing the tendency to skipped beats. When my heartbeat rate is trying to increase it is plagued by premature beats every other beat and so skips alternate beats resulting in a pulse rate half of normal, eg after mild exertion a pulse of 40/min, when it is trying to make 80. This does not help getting blood to my head when OI is in effect due to changing body orientation and heart to head angle changes from horizontal to vertical.
Mij
Senior Member (Voting Rights)
I will have to check whether I have already post in this thread but just while I remember a few things I found it really hard for years to move my head quick enough to cross a road. It felt like my head was filled with fluid and turning my head from side to side made me off balance and my gait would try to steady myself.
I've experienced this too for many years. I refer to it as 'vestibular gait' and not OI related, including legs standing apart in the shower to hold my balance. The shower water pouring on my head might be related to both OI and vestibular imbalances.
Liie
Senior Member (Voting Rights)
I have the objective signs of POTS, that is, raised hearth rate by more than 30 BPM when going from lying down to standing. But I don't have any clear subjective symptoms. No vertigo or dizziness or unpleasant palpitations or feeling like I'm about to faint. So the condition doesn't bother me at all in any clear way.
However I'm thinking that maybe the raised heart rate contribute to why I feel tired fast when I am standing or walking. I am lucky to have pretty high physical endurance compared to many people with ME/CFS, I can be active on my feet for maybe 20-30 minutes without any problems. But after about that amount of time it gets harder and harder to remain upright, even without any activity. It feels like hard effort just to keep standing, like if I had run a marathon and just need to lay down. For a long time I thought that this is just because of low energy level in general, but maybe POTS contributes a little or a lot.
Are there other forum members who recognise this?
Do anyone have experience with medication that has made it easier to remain upright for a longer time? For example pyridostigmine, fludrocortisone, ivabradine or beta blockers? I tried a beta blocker, but although it lowered my blood pressure and heart-rate it didn't significantly lower the raise in heart rate when standing or made it easier to remain upright for a longer time.
I'm thinking about whether it's worth the effort to pursue a prescription some medication for POTS, and the experience of other people who have found that it helps them to remain upright would be interesting to hear about.
However I'm thinking that maybe the raised heart rate contribute to why I feel tired fast when I am standing or walking. I am lucky to have pretty high physical endurance compared to many people with ME/CFS, I can be active on my feet for maybe 20-30 minutes without any problems. But after about that amount of time it gets harder and harder to remain upright, even without any activity. It feels like hard effort just to keep standing, like if I had run a marathon and just need to lay down. For a long time I thought that this is just because of low energy level in general, but maybe POTS contributes a little or a lot.
Are there other forum members who recognise this?
Do anyone have experience with medication that has made it easier to remain upright for a longer time? For example pyridostigmine, fludrocortisone, ivabradine or beta blockers? I tried a beta blocker, but although it lowered my blood pressure and heart-rate it didn't significantly lower the raise in heart rate when standing or made it easier to remain upright for a longer time.
I'm thinking about whether it's worth the effort to pursue a prescription some medication for POTS, and the experience of other people who have found that it helps them to remain upright would be interesting to hear about.
Last edited:
I will have to check whether I have already post in this thread but just while I remember a few things I found it really hard for years to move my head quick enough to cross a road. It felt like my head was filled with fluid and turning my head from side to side made me off balance and my gait would try to steady myself.
I also went through a period at very severe ME where my neck and spine felt like jelly. I caught hardly hold my head up or sit upright.
I had what I think is a similar sensation at onset. If I turned my head to left or right it felt as if (the back of) my brain was continuing to rotate past its centre-line. It was completely bizarre and a novel sensation, not really like vertigo though. I think I mentioned this in past years but can't find it if I did.
Also, it's a new year and based on the past year my phone has just reminded me to "be careful out there". Great.
Utsikt
Senior Member (Voting Rights)
Sounds like my OI experiences. I had the same when I was moderate, and it just got a lot worse when I became severe.But after about that amount of time it gets harder and harder to remain upright, even without any activity. It feels like hard effort just to keep standing, like if I had run a marathon and just need to lay down. For a long time I thought that this is just because of low energy level in general, but maybe POTS contributes a little or a lot.
Are there other forum members who recognise this?
Kitty
Senior Member (Voting Rights)
Also, it's a new year and based on the past year my phone has just reminded me to "be careful out there".
When I updated my phone, the OS kept triggering an alarm that made the handset vibrate and beep insistently, with the screen showing a big message saying press the side button to call the emergency services.
The motion sensor was showing I'd fallen, even though I'd only reached down to get something out of the dishwasher or got up from a sitting position. Presumably it's because my gait's all over the place, I stagger and lose balance and walk into things all the time. I had to turn the feature off permanently, it was being triggered two or three times a day.
I've also had the egg yolk brain sensation. I'm not sure, but I wonder if it's something to do with eye tracking, or maybe the bit of the brain that predicts eye movement. I've never had it when I've been stable, only ever when I'm really ill and exhausted.
StellariaGraminea
Senior Member (Voting Rights)
I can be active on my feet for maybe 20-30 minutes without any problems. But after about that amount of time it gets harder and harder to remain upright, even without any activity. It feels like hard effort just to keep standing, like if I had run a marathon and just need to lay down. For a long time I thought that this is just because of low energy level in general, but maybe POTS contributes a little or a lot.
Are there other forum members who recognise this?
Yes, I have the same (but varies from bad periods where 2-3 minutes on my feet I reach this stage to good periods where I could be 15 minutes on feet moving around as long as it's not too vigorous). But both sitting / standing have a similar effect when I reach that stage, I just have to get horizontal. If I rest before the feeling that blood is draining out of my head, I can rest for a short time e.g. 5 mins and get up again and repeat the upright activity. But if I push through, even only a few minutes extra, it could be hours before I recover.
The worst was two different times I had to be upright for several hours for a medical appt. I could feel that blood draining out of my brain feeling but couldn't do anything about it. Yes, of course, I could have laid on the floor in the GP's surgery... but with these illnesses you're already painful anticipating gaslighting and I didn't want to appear like the "hysterical" patient & lose anymore credibility. I suffered for it then and hours after.
The second time was much much worse, also longer than the GP visit. It took months to recover and I never again want to experience the level of suffering I went through. This is where I've questions re the overlap between pots-like conditions / ME. My reaction in the 2nd one ticked all the boxes for PEM but I wonder can it be explained by lack of brain blood flow. The characteristic feeling I get is hard to explain but it feels like my brain is being deprived of blood.
Do anyone have experience with medication that has made it easier to remain upright for a longer time?
Yes this was the most important effect of ivabradine for me. (Yes, it normalised my excessive HR when upright, but tbh I couldn't feel my HR and that didn't bother me). Ivab. brought me (on second day of use) from being able to sit up about ~1-5mins before urgently having to lie down, to being able to sit up and talk for e.g. half an hour in a casual conversation. I've no idea why but it seemed to help my voice too... energy or air to speak. My voice used to run out after a couple sentences, but with ivabradine I could just talk longer. V noticeable. Wasn't expecting that effect.
My underlying POTS has improved a lot several years in though, so the benefits of ivabradine are less dramatic & may not be necessary anymore, am looking at stopping it.
AliceLily
Senior Member (Voting Rights)
Thanks Mij. I wouldn't be surprised if it was a separate thing from the OI. I had so much going on it wasn't funny. I also have POTS like symptoms. I had mentioned about shower thing a number of times and I don't think anyone apart from you had the same problem with needing to place the feet wide apart just to try to keep a balance in the shower. So I in future I might look at that side of it as another awful symptom I have to deal with.I've experienced this too for many years. I refer to it as 'vestibular gait' and not OI related, including legs standing apart in the shower to hold my balance. The shower water pouring on my head might be related to both OI and vestibular imbalances.
AliceLily
Senior Member (Voting Rights)
It does sound like you experienced the same thing. And you are right in that it wasn't vertigo in the way that makes you be sick. Mine has improved but it is still there.I had what I think is a similar sensation at onset. If I turned my head to left or right it felt as if (the back of) my brain was continuing to rotate past its centre-line. It was completely bizarre and a novel sensation, not really like vertigo though. I think I mentioned this in past years but can't find it if I did.
Also, it's a new year and based on the past year my phone has just reminded me to "be careful out there". Great.
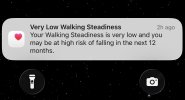
View attachment 30000
Yes, I could be vulnerable to falls the older I get because of it. I get through 5-6 liters of milk each week so hoping that will keep my bones from breaking if I do have any falls. I haven't had a broken bone yet, 62 years now.
Liie
Senior Member (Voting Rights)
Sounds like my OI experiences.
Thanks for your input! It's interesting to hear that your experiences are similar. I will start taking huperzine supplements shortly. If that doesn't help I will try to get a prescription for pyridostigmine or ivabradine.Yes, I have the same.
