“The burden of post-acute COVID-19 symptoms in a multinational network cohort analysis”
Kostka, Kristin; Roel, Elena; Trinh, Nhung T. H.; Mercadé-Besora, Núria; Delmestri, Antonella; Mateu, Lourdes; Paredes, Roger; Duarte-Salles, Talita; Prieto-Alhambra, Daniel; Català, Martí; Jödicke, Annika M.
Persistent symptoms following the acute phase of COVID-19 present a major burden to both the affected and the wider community.
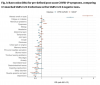
We conducted a cohort study including over 856,840 first COVID-19 cases, 72,422 re-infections and more than 3.1 million first negative-test controls from primary care electronic health records from Spain and the UK (Sept 2020 to Jan 2022 (UK)/March 2022 (Spain)). We characterised post-acute COVID-19 symptoms and identified key symptoms associated with persistent disease. We estimated incidence rates of persisting symptoms in the general population and among COVID-19 patients over time. Subsequently, we investigated which WHO-listed symptoms were particularly differential by comparing their frequency in COVID-19 cases vs. matched test-negative controls. Lastly, we compared persistent symptoms after first infections vs. reinfections.
Our study shows that the proportion of COVID-19 cases affected by persistent post-acute COVID-19 symptoms declined over the study period. Risk for altered smell/taste was consistently higher in patients with COVID-19 vs test-negative controls. Persistent symptoms were more common after reinfection than following a first infection.
More research is needed into the definition of long COVID, and the effect of interventions to minimise the risk and impact of persistent symptoms.
Link | PDF (Nature Communications)
Kostka, Kristin; Roel, Elena; Trinh, Nhung T. H.; Mercadé-Besora, Núria; Delmestri, Antonella; Mateu, Lourdes; Paredes, Roger; Duarte-Salles, Talita; Prieto-Alhambra, Daniel; Català, Martí; Jödicke, Annika M.
Persistent symptoms following the acute phase of COVID-19 present a major burden to both the affected and the wider community.
We conducted a cohort study including over 856,840 first COVID-19 cases, 72,422 re-infections and more than 3.1 million first negative-test controls from primary care electronic health records from Spain and the UK (Sept 2020 to Jan 2022 (UK)/March 2022 (Spain)). We characterised post-acute COVID-19 symptoms and identified key symptoms associated with persistent disease. We estimated incidence rates of persisting symptoms in the general population and among COVID-19 patients over time. Subsequently, we investigated which WHO-listed symptoms were particularly differential by comparing their frequency in COVID-19 cases vs. matched test-negative controls. Lastly, we compared persistent symptoms after first infections vs. reinfections.
Our study shows that the proportion of COVID-19 cases affected by persistent post-acute COVID-19 symptoms declined over the study period. Risk for altered smell/taste was consistently higher in patients with COVID-19 vs test-negative controls. Persistent symptoms were more common after reinfection than following a first infection.
More research is needed into the definition of long COVID, and the effect of interventions to minimise the risk and impact of persistent symptoms.
Link | PDF (Nature Communications)