From a bad patch then, generally, the Likert scores are the first to react to any improvement. Then, once the overall score has been improved, the changes occur both up the Likert scale and across the Bimodal scale (although you will also see that there are many in the second phase still trying to move up out of the depths of the pit in the bottom left corner). This is very difficult to explain in words, because the relationship between the two scoring methods is not simple.
Using the medians as averages, we can say that the Likert score needs to improve by 8 points before the Bimodal score starts to change by 1 or 2 points: an improvement of 10 on the Likert matches a move of 3 across on the Bimodal score, 12 up for an improvement of 4 across and 15 up for an improvement of 5 across.
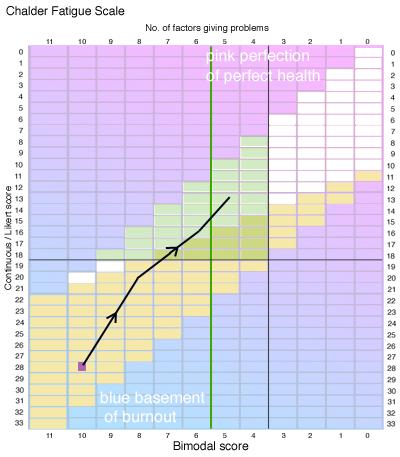 Here is a specific example of what that means. If a person is towards the bottom left corner at 10/28 (shown as a purple square), then the black line represents the average improvement pattern (although of course, only a few improve by as much as this). To satisfy the original criterion in the protocol document, that person would have to halve the bimodal score to 5, which is where the black line ends. Here is a specific example of what that means. If a person is towards the bottom left corner at 10/28 (shown as a purple square), then the black line represents the average improvement pattern (although of course, only a few improve by as much as this). To satisfy the original criterion in the protocol document, that person would have to halve the bimodal score to 5, which is where the black line ends.
But you can also see that long before then, the person would cross the horizontal line at 18, which was the final criterion used by PACE to measure a "return to normal function": clearly a much easier target. Not only that, but the person would still be to the left of the green line and still be ill enough to qualify for inclusion into the PACE trial all over again.
In fact this situation (where it is much easier to satisfy the final target of 18 than the original requirement of halving the bimodal score) would be true for every position on the grid for patients. (However, we have too little data in from our survey to make a fair comment regarding movement from the bottom two places in the Bimodal 11 column.)
|