Remotely delivered weight management for people with long COVID and overweight: the randomized wait-list-controlled ReDIRECT trial
Emilie Combet, Laura Haag, Janice Richardson, Caroline E. Haig, Yvonne Cunningham, Heather L. Fraser, Naomi Brosnahan, Tracy Ibbotson, Jane Ormerod, Chris White, Emma McIntosh, Catherine A. O’Donnell, Naveed Sattar, Alex McConnachie, Michael E. J. Lean & David N. Blane
[Line breaks added]
Abstract
Long COVID (LC) is a complex multisymptom condition with no known disease-modifying treatments. This wait-list-controlled open-label trial tested whether a remotely delivered structured weight management program could improve respective LC symptoms in people living with overweight.
Adults with LC (symptoms >12 weeks) and body mass index >27 kg m−2 (>25 kg m−2 for South Asians) were randomized (n = 234, 1:1) to control (n = 116, usual care) or the remotely delivered structured weight management (n = 118, total diet replacement (850 kcal per day) for 12 weeks, followed by food reintroduction and weight loss maintenance support) via minimization and randomization (80:20) to balance dominant LC symptom, sex, age, ethnicity and postcode-based index of multiple deprivation between groups. The control group received the intervention after 6 months.
Participants selected the dominant LC symptom they would most like to improve (fatigue, breathlessness, pain, anxiety/depression or other) as the prespecified respective primary outcome. Individual symptoms were assessed using validated questionnaires and a visual analog scale for those without prespecified scales.
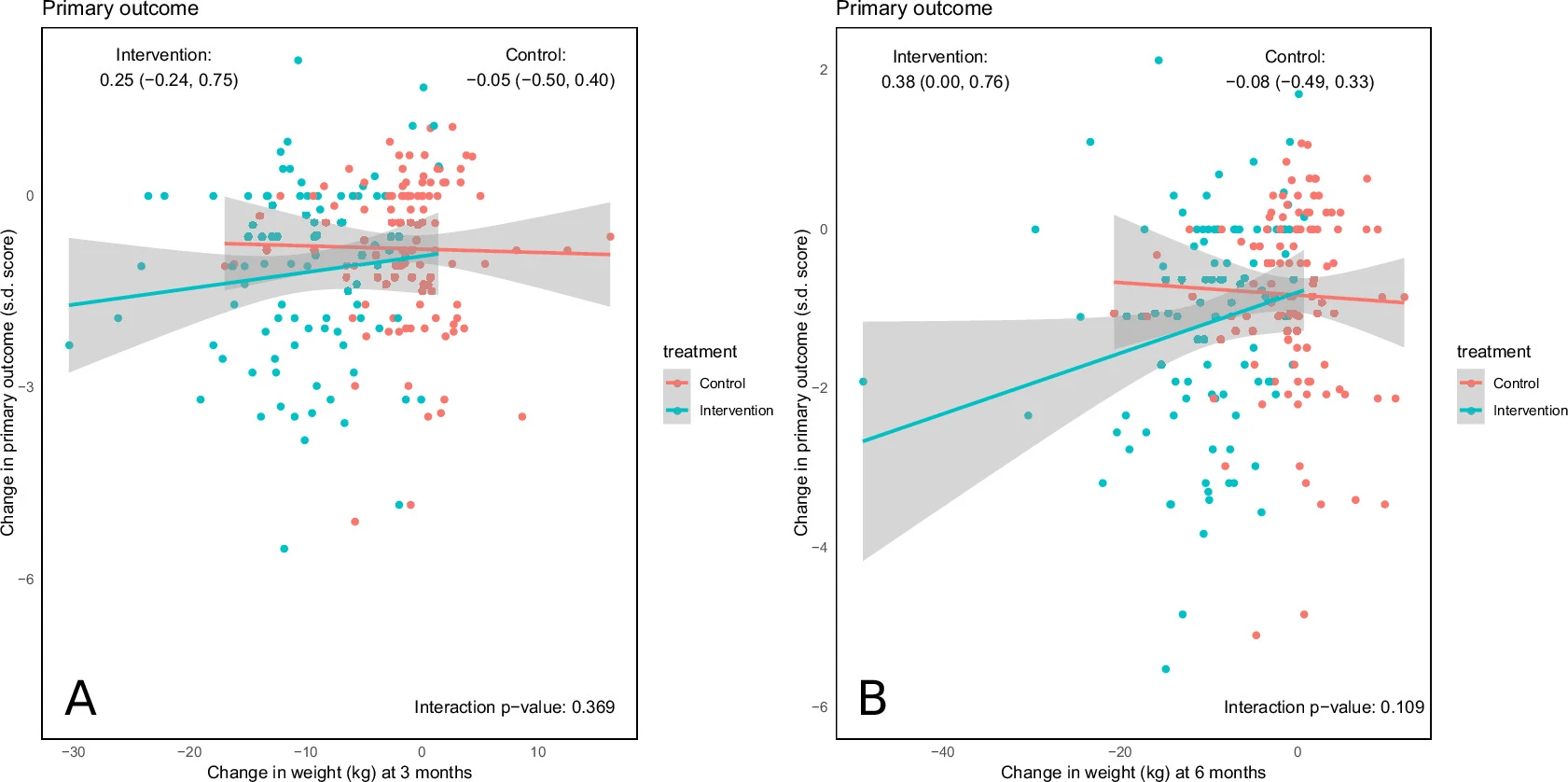
At 6 months, the primary outcome improved in the intervention group (change −1.16 (s.d. 1.42), n = 97 analyzed) compared with the control group (change −0.83 (s.d. 1.14), n = 117 analyzed) with a treatment effect of −0.34 (95% confidence interval −0.67 to −0.01), with no excess of serious adverse events.
Link | PDF (Nature Medicine) [Open Access]
Emilie Combet, Laura Haag, Janice Richardson, Caroline E. Haig, Yvonne Cunningham, Heather L. Fraser, Naomi Brosnahan, Tracy Ibbotson, Jane Ormerod, Chris White, Emma McIntosh, Catherine A. O’Donnell, Naveed Sattar, Alex McConnachie, Michael E. J. Lean & David N. Blane
[Line breaks added]
Abstract
Long COVID (LC) is a complex multisymptom condition with no known disease-modifying treatments. This wait-list-controlled open-label trial tested whether a remotely delivered structured weight management program could improve respective LC symptoms in people living with overweight.
Adults with LC (symptoms >12 weeks) and body mass index >27 kg m−2 (>25 kg m−2 for South Asians) were randomized (n = 234, 1:1) to control (n = 116, usual care) or the remotely delivered structured weight management (n = 118, total diet replacement (850 kcal per day) for 12 weeks, followed by food reintroduction and weight loss maintenance support) via minimization and randomization (80:20) to balance dominant LC symptom, sex, age, ethnicity and postcode-based index of multiple deprivation between groups. The control group received the intervention after 6 months.
Participants selected the dominant LC symptom they would most like to improve (fatigue, breathlessness, pain, anxiety/depression or other) as the prespecified respective primary outcome. Individual symptoms were assessed using validated questionnaires and a visual analog scale for those without prespecified scales.
At 6 months, the primary outcome improved in the intervention group (change −1.16 (s.d. 1.42), n = 97 analyzed) compared with the control group (change −0.83 (s.d. 1.14), n = 117 analyzed) with a treatment effect of −0.34 (95% confidence interval −0.67 to −0.01), with no excess of serious adverse events.
Link | PDF (Nature Medicine) [Open Access]