Post-COVID-19 condition in prospective inpatient and outpatient cohorts
Antti Hurme, Arja Viinanen, Johanna Teräsjärvi, Pinja Jalkanen, Thijs Feuth, Eliisa Löyttyniemi, Tytti Vuorinen, Anu Kantele, Jarmo Oksi, Qiushui He, Ilkka Julkunen
[Line breaks added]
Abstract
Viral persistence, immune dysregulation, hypocortisolism, and pulmonary tissue damage from acute infection are proposed as pathogenic mechanisms underlying post-COVID-19 condition (PCC).
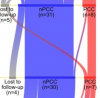
In this prospective observational study, we followed 62 COVID-19 inpatients and 53 COVID-19 outpatients for 24 months after the infection. During this period, we assessed prolonged symptoms, lung function, and a set of immunological markers and a proportion of the patient group was assessed with computed tomography three months post-infection.
The prevalence of PCC, as assessed by four medical specialists, decreased from 51% at three months to 18% at 24 months. Risk factors included the severity of the acute infection and comorbidities of obstructive sleep apnea or obesity. Patients with PCC had higher serum levels of anti-SARS-CoV-2 S1 and N protein antibodies.
In the whole group, spirometry results, orthostatic hypotension, or levels of soluble suppression of tumorigenicity 2, interleukin 6 (IL-6), high-sensitivity C-reactive protein (hs-CRP), or cortisol had no association with PCC. However, using symptom clusters, patients with cognitive problems had lower cortisol levels, while patients with ongoing respiratory or myalgic symptoms had higher levels of IL-6 and hs-CRP. However, more extensive studies with clustering are needed to validate these results.
Link | PDF (Scientific Reports) [Open Access]
Antti Hurme, Arja Viinanen, Johanna Teräsjärvi, Pinja Jalkanen, Thijs Feuth, Eliisa Löyttyniemi, Tytti Vuorinen, Anu Kantele, Jarmo Oksi, Qiushui He, Ilkka Julkunen
[Line breaks added]
Abstract
Viral persistence, immune dysregulation, hypocortisolism, and pulmonary tissue damage from acute infection are proposed as pathogenic mechanisms underlying post-COVID-19 condition (PCC).
In this prospective observational study, we followed 62 COVID-19 inpatients and 53 COVID-19 outpatients for 24 months after the infection. During this period, we assessed prolonged symptoms, lung function, and a set of immunological markers and a proportion of the patient group was assessed with computed tomography three months post-infection.
The prevalence of PCC, as assessed by four medical specialists, decreased from 51% at three months to 18% at 24 months. Risk factors included the severity of the acute infection and comorbidities of obstructive sleep apnea or obesity. Patients with PCC had higher serum levels of anti-SARS-CoV-2 S1 and N protein antibodies.
In the whole group, spirometry results, orthostatic hypotension, or levels of soluble suppression of tumorigenicity 2, interleukin 6 (IL-6), high-sensitivity C-reactive protein (hs-CRP), or cortisol had no association with PCC. However, using symptom clusters, patients with cognitive problems had lower cortisol levels, while patients with ongoing respiratory or myalgic symptoms had higher levels of IL-6 and hs-CRP. However, more extensive studies with clustering are needed to validate these results.
Link | PDF (Scientific Reports) [Open Access]