Chandelier
Senior Member (Voting Rights)
Persistent Immune Dysregulation during Post-Acute Sequelae of COVID-19 is Manifested in Antibodies Targeting Envelope and Nucleocapsid Proteins
Abstract
Post-Acute Sequelae of SARS-CoV-2 infection (PASC) syndrome or “Long COVID” represents a widespread health challenge that necessitates the development of novel diagnostic approaches and targeted therapies that can be readily deployed.Immune dysregulation has been reported as one of the hallmarks of PASC, but the extent of PASC immune dysregulation in patients over time remains unclear.
We therefore assessed SARS-CoV-2-specific antibody responses, peripheral immune cell profiles, autoantibody profiles and circulating cytokines for up to 6 months in participants with a SARS-CoV-2 infection who either convalesced or developed PASC.
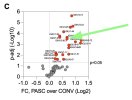
Compared to convalescent, PASC participants with a broad range of PASC phenotypes exhibited persistently elevated IgG titers for SARS-CoV-2 Envelope and Nucleocapsid proteins over the 6 months of study duration.
In contrast, the IgG responses to Spike protein were significantly lower in the PASC cohort with predominantly IgG1 and IgG3 class-switched bias. Using CyTOF analysis, we show elevated numbers of circulating T follicular helper cells (cTFH) and mucosa-associated invariant T cells (MAIT), which also correlated with high anti-Envelope IgG titers.
Persistent immune activation was accompanied by augmented serum cytokine profiles with LIF, IL-11, Eotaxin-3, and HMGB-1 in PASC participants, who also demonstrated significantly higher rates of autoantibodies.
These findings highlight the persistence of immune dysregulation in PASC, underscoring the need to explore targeted therapies addressing viral persistence, dysregulated antibody production, and autoimmunity.
Competing Interest Statement
Jerry A. Krishnan, MD, PhD, reports grants from National Institutes of Health during the conduct of the study; research grants from the American Lung Association, BioVie Pharma, COPD Foundation, and Patient Centered Outcomes Research Institute outside the submitted work; and personal fees from AstraZeneca, Inogen, MedImmune, RespirAI, and Verona Pharma.Marcin Kwissa, Manikannan Mathayan, Satyajeet S. Salunkhe, Velavan Bakthavachalam, Zijing Ye, Mark A. Sanborn, Samantha Condo, Aditi Upadhye, Athulith Nemakal, Justin M. Richner, Sanjib Basu, Richard M. Novak, Jeffrey R. Jacobson, Balaji B Ganesh, Martha Cerda, Paul J. Utz, Jerry A. Krishnan, Bellur S. Prabhakar, Jalees Rehman