Long-Term Adverse Effects of Mild COVID-19 Disease on Arterial Stiffness, and Systemic and Central Hemodynamics: A Pre-Post Study
Podrug, Mario; Koren, Pjero; Dražić Maras, Edita; Podrug, Josip; Čulić, Viktor; Perissiou, Maria; Bruno, Rosa Maria; Mudnić, Ivana; Boban, Mladen; Jerončić, Ana
COVID-19-associated vascular disease complications are primarily associated with endothelial dysfunction; however, the consequences of disease on vascular structure and function, particularly in the long term (>7 weeks post-infection), remain unexplored.
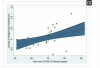
Individual pre and post-infection changes in arterial stiffness as well as central and systemic hemodynamic parameters were measured in patients diagnosed with mild COVID-19. As part of in-laboratory observational studies, baseline measurements were taken up to two years before, whereas the post-infection measurements were made 2–3 months after the onset of COVID-19. We used the same measurement protocol throughout the study as well as linear and mixed-effects regression models to analyze the data. Patients (N = 32) were predominantly healthy and young (mean age ± SD: 36.6 ± 12.6).
We found that various parameters of arterial stiffness and central hemodynamics—cfPWV, AIx@HR75, and cDBP as well as DBP and MAP—responded to a mild COVID-19 disease. The magnitude of these responses was dependent on the time since the onset of COVID-19 as well as age (pregression_models ≤ 0.013). In fact, mixed-effects models predicted a clinically significant progression of vascular impairment within the period of 2–3 months following infection (change in cfPWV by +1.4 m/s, +15% in AIx@HR75, approximately +8 mmHg in DBP, cDBP, and MAP).
The results point toward the existence of a widespread and long-lasting pathological process in the vasculature following mild COVID-19 disease, with heterogeneous individual responses, some of which may be triggered by an autoimmune response to COVID-19.
Link | PDF (Journal of Clinical Medicine)
Podrug, Mario; Koren, Pjero; Dražić Maras, Edita; Podrug, Josip; Čulić, Viktor; Perissiou, Maria; Bruno, Rosa Maria; Mudnić, Ivana; Boban, Mladen; Jerončić, Ana
COVID-19-associated vascular disease complications are primarily associated with endothelial dysfunction; however, the consequences of disease on vascular structure and function, particularly in the long term (>7 weeks post-infection), remain unexplored.
Individual pre and post-infection changes in arterial stiffness as well as central and systemic hemodynamic parameters were measured in patients diagnosed with mild COVID-19. As part of in-laboratory observational studies, baseline measurements were taken up to two years before, whereas the post-infection measurements were made 2–3 months after the onset of COVID-19. We used the same measurement protocol throughout the study as well as linear and mixed-effects regression models to analyze the data. Patients (N = 32) were predominantly healthy and young (mean age ± SD: 36.6 ± 12.6).
We found that various parameters of arterial stiffness and central hemodynamics—cfPWV, AIx@HR75, and cDBP as well as DBP and MAP—responded to a mild COVID-19 disease. The magnitude of these responses was dependent on the time since the onset of COVID-19 as well as age (pregression_models ≤ 0.013). In fact, mixed-effects models predicted a clinically significant progression of vascular impairment within the period of 2–3 months following infection (change in cfPWV by +1.4 m/s, +15% in AIx@HR75, approximately +8 mmHg in DBP, cDBP, and MAP).
The results point toward the existence of a widespread and long-lasting pathological process in the vasculature following mild COVID-19 disease, with heterogeneous individual responses, some of which may be triggered by an autoimmune response to COVID-19.
Link | PDF (Journal of Clinical Medicine)