Health outcomes in hospitalised and non-hospitalised individuals after COVID-19, an observational, cross-sectional study
BACKGROUND
Both hospitalised (H) and non-hospitalised (NH) individuals may have different symptoms and impairments after COVID-19. We aimed to explore symptoms, mental and physical health after initial COVID-19 for both groups of individuals and the association between physical and mental impairments in relation to self-rated health status and to identify different cluster profiles.
METHODS
Participants were recruited between June 2020 until December 2022 at the Karolinska University Hospital, Sweden. Data was collected at first assessment after COVID-19 and consisted of demographics, medical history, symptoms and results from physical function tests and self-reported questionnaires.
RESULTS
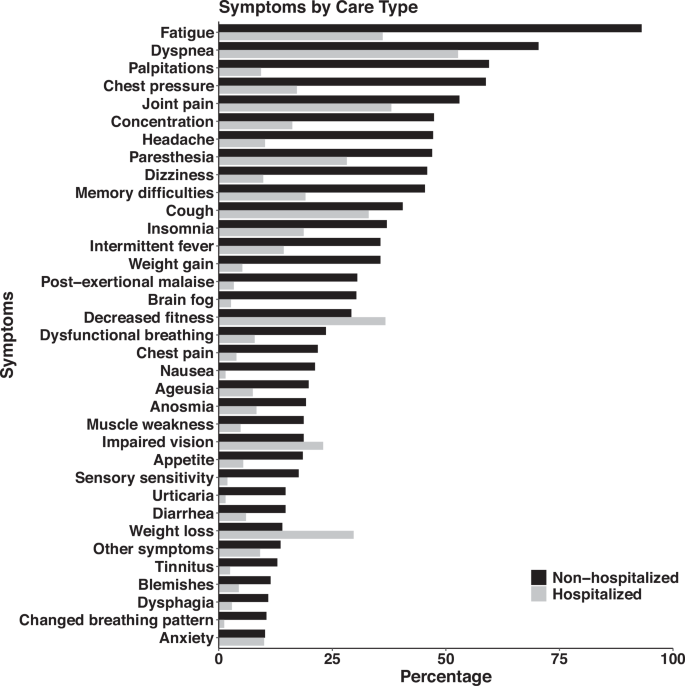
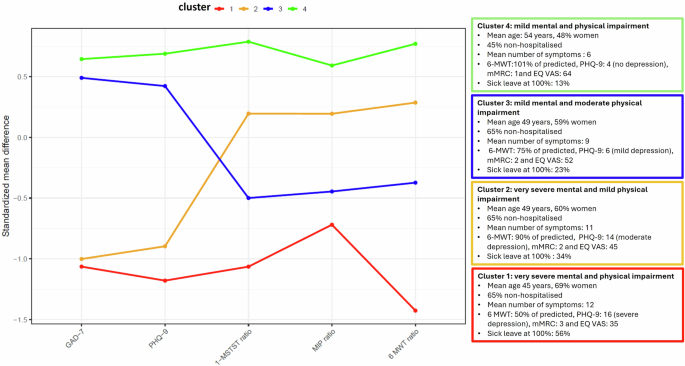
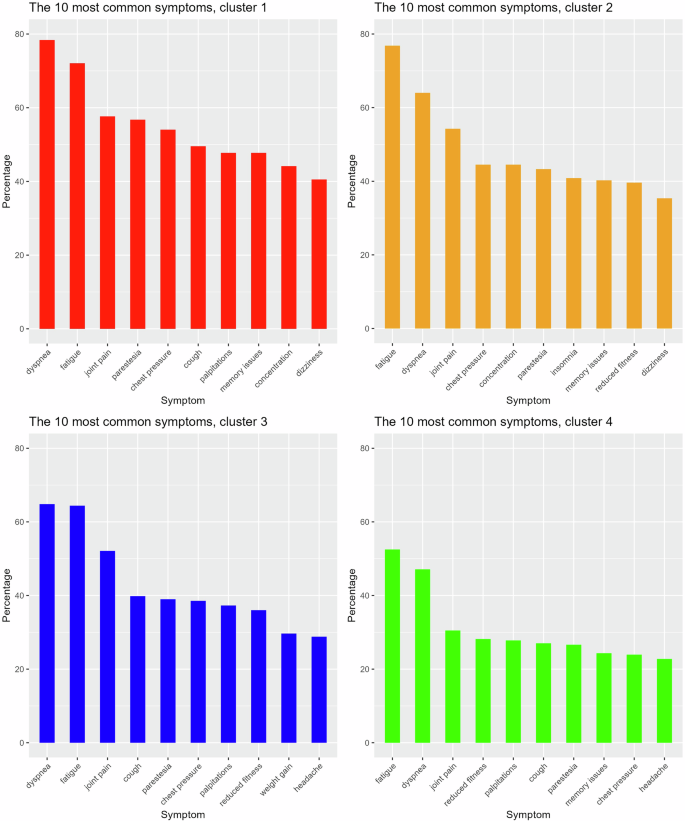
Here we show that among 931 participants, the H-group are older (mean age 56.7 years) and predominantly male (72%), while the NH-group are younger (mean age 44.4 years) and mostly female (84%). Fatigue, dyspnoea, joint pain, paraesthesia, and chest pressure are common symptoms reported across all participants. Physical function is lower than predicted in both groups and the NH-group have higher prevalence of depression and fatigue. These impairments together with dyspnoea, number of symptoms and sick leave are also associated with reduced self-rated health. Four specific cluster profiles have been identified, and 66.4% of the participants have severe to moderate impairments.
CONCLUSIONS
Regardless of the initial level of care approximately two-thirds of the participants exhibit various physical and mental impairments associated to self-rated health after COVID-19. We propose that defining specific cluster profiles is crucial for tailoring management of post-COVID sequelae. Further long-term studies are needed to understand recovery trajectories to optimise targeted interventions.
PLAIN LANGUAGE SUMMARY
This study examined symptom burden and physical and mental impairments in individuals with post–COVID-19 condition (PCC), comparing those who had been hospitalised with those who had not. Data from 931 participants (July 2020–December 2022) included medical history, physical tests, and questionnaires. Fatigue, breathlessness, joint pain, tingling, and chest pressure were common. Both groups showed reduced physical function, while depression and fatigue were more prevalent among non-hospitalised individuals. Four cluster profiles were identified, with most participants reporting moderate to severe impairments affecting self-rated health. These findings underscore the importance of comprehensive assessment and long-term follow-up to support recovery and guide rehabilitation strategies for people living with PCC.
Web | DOI | PDF | Nature Communications Medicine | Open Access
Nygren-Bonnier, Malin; Svensson-Raskh, Anna; Holmström, Linda; Törnberg, Anna; Svensson, Annie; Loewenstein, Daniel; Regardt, Malin; Björnson, Mikael; Hallberg, Carl; Kemani, Mike; Mc Allister, Anita; Körner Gustafsson, Joakim; Halvarsson, Alexandra; Ekman, Urban; Nordstrand, Linda; Guidetti, Susanne; Anmyr, Lena; Bragesjö, Maria; Åström Reitan, Jenny; Badinlou, Farzaneh; Dahl, Oili; Åkerman, Eva; Villner, Pär; Brodin, Petter; Caidahl, Kenneth; Ståhlberg, Marcus; Fedorowski, Artur; Sköld, Magnus; Runold, Michael; Bruchfeld, Judith; Rydwik, Elisabeth
BACKGROUND
Both hospitalised (H) and non-hospitalised (NH) individuals may have different symptoms and impairments after COVID-19. We aimed to explore symptoms, mental and physical health after initial COVID-19 for both groups of individuals and the association between physical and mental impairments in relation to self-rated health status and to identify different cluster profiles.
METHODS
Participants were recruited between June 2020 until December 2022 at the Karolinska University Hospital, Sweden. Data was collected at first assessment after COVID-19 and consisted of demographics, medical history, symptoms and results from physical function tests and self-reported questionnaires.
RESULTS
Here we show that among 931 participants, the H-group are older (mean age 56.7 years) and predominantly male (72%), while the NH-group are younger (mean age 44.4 years) and mostly female (84%). Fatigue, dyspnoea, joint pain, paraesthesia, and chest pressure are common symptoms reported across all participants. Physical function is lower than predicted in both groups and the NH-group have higher prevalence of depression and fatigue. These impairments together with dyspnoea, number of symptoms and sick leave are also associated with reduced self-rated health. Four specific cluster profiles have been identified, and 66.4% of the participants have severe to moderate impairments.
CONCLUSIONS
Regardless of the initial level of care approximately two-thirds of the participants exhibit various physical and mental impairments associated to self-rated health after COVID-19. We propose that defining specific cluster profiles is crucial for tailoring management of post-COVID sequelae. Further long-term studies are needed to understand recovery trajectories to optimise targeted interventions.
PLAIN LANGUAGE SUMMARY
This study examined symptom burden and physical and mental impairments in individuals with post–COVID-19 condition (PCC), comparing those who had been hospitalised with those who had not. Data from 931 participants (July 2020–December 2022) included medical history, physical tests, and questionnaires. Fatigue, breathlessness, joint pain, tingling, and chest pressure were common. Both groups showed reduced physical function, while depression and fatigue were more prevalent among non-hospitalised individuals. Four cluster profiles were identified, with most participants reporting moderate to severe impairments affecting self-rated health. These findings underscore the importance of comprehensive assessment and long-term follow-up to support recovery and guide rehabilitation strategies for people living with PCC.
Web | DOI | PDF | Nature Communications Medicine | Open Access