Abstract
Mitochondrial dysfunction and stem cell exhaustion contribute to age-related immune decline, yet clinical interventions targeting immune aging are lacking. Recently, we demonstrated that urolithin A (UA), a mitophagy inducer, expands T memory stem cells (TSCM) and naive T cells in mice. In this randomized, double-blind, placebo-controlled trial, 50 healthy middle-aged adults received oral UA (1,000 mg day−1) or placebo for 4 weeks; time points of analysis were baseline and day 28. Primary outcomes were phenotypical changes in peripheral CD3+ T cell subsets and immune metabolic remodeling. UA expanded peripheral naive-like, less terminally exhausted CD8+ cells (treatment difference 0.50 percentage points; 95% CI = 0.16 to 0.83; P = 0.0437) while also increasing CD8+fatty acid oxidation capacity (treatment difference = 14.72 percentage points; 95% confidence interval (CI) = 6.46 to 22.99; P = 0.0061). Secondary outcomes included changes in plasma cytokine levels (IL-6, TNF, IL-1β, IL-10), immune populations assessed via flow cytometry, immune cell function, and mitochondrial content. Analysis revealed augmented mitochondrial biogenesis in CD8+ cells, increased peripheral CD56dimCD16bright NK cells, and nonclassical CD14loCD16hi monocytes in UA-treated participants, as well as improved activation-elicited TNF secretion in T cells and bacterial uptake by monocytes. Exploratory single-cell RNA sequencing demonstrated UA-driven transcriptional shifts across immune populations, modulating pathways linked to inflammation and metabolism. These findings indicate that short-term UA supplementation modulates human immune cell composition and function, supporting its potential to counteract age-related immune decline and inflammaging. ClinicalTrials.gov registration number: NCT05735886.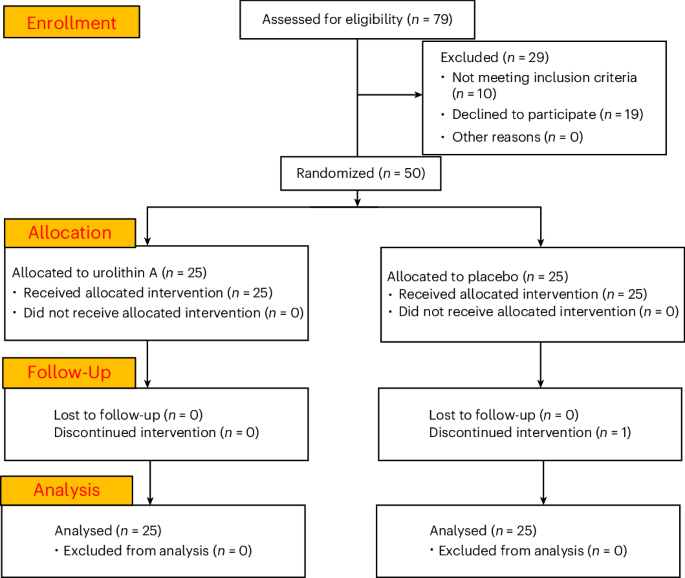
Effect of the mitophagy inducer urolithin A on age-related immune decline: a randomized, placebo-controlled trial - Nature Aging
Immune aging fosters multimorbidity and compromises control of infection and cancer. In a phase 1 randomized controlled trial in middle-aged adults, Denk and colleagues administer the mitophagy inducer urolithin A and profile cellular and metabolic aspects of immune aging.
